This document discusses tonsillitis, tonsillectomy, and adenoidectomy. It provides details on:
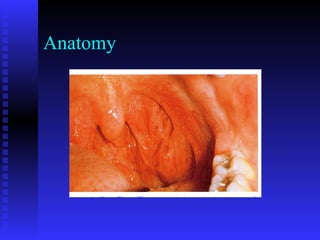
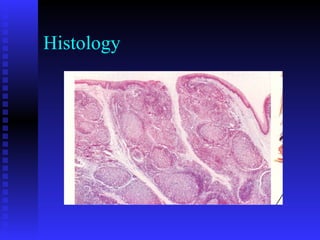
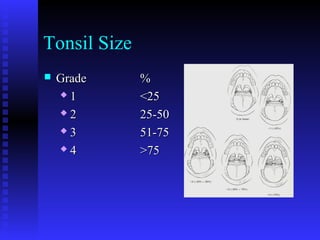
- The history and anatomy of these procedures
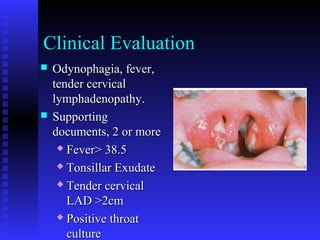
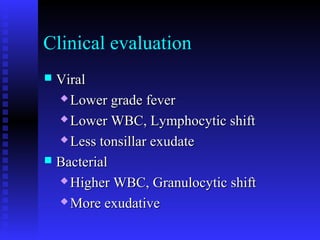
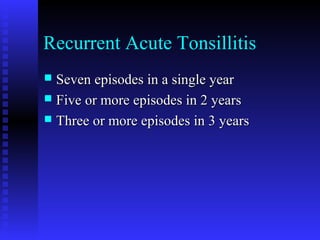
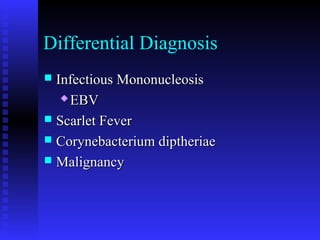
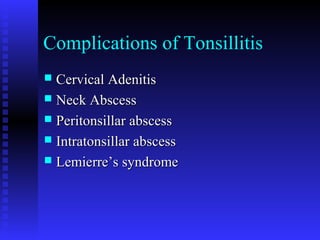
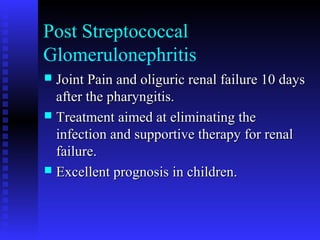
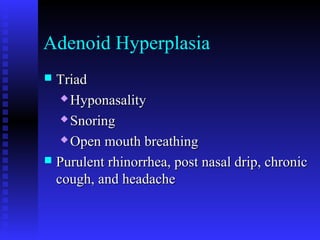
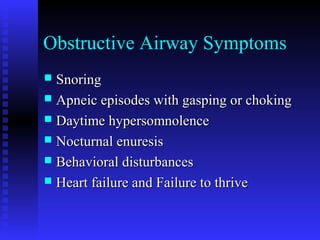
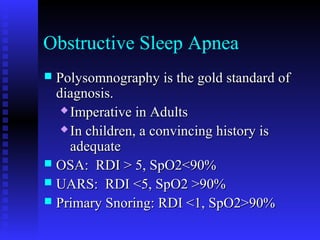
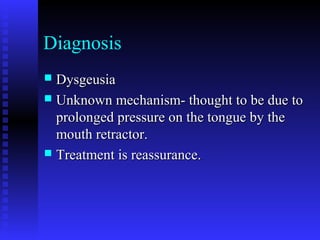
- Clinical evaluation and differential diagnosis of tonsillitis
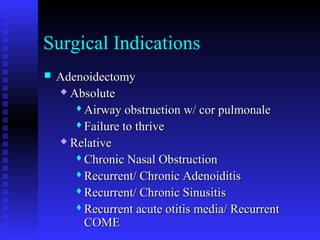
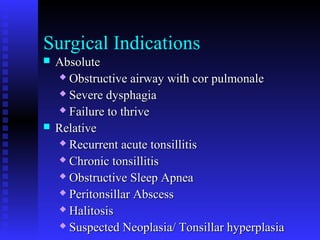
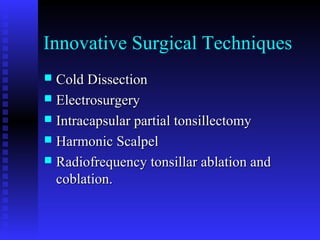
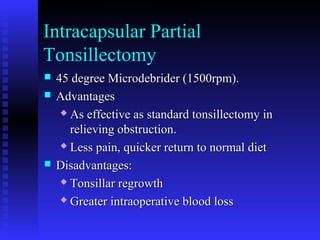
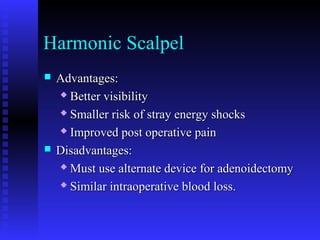
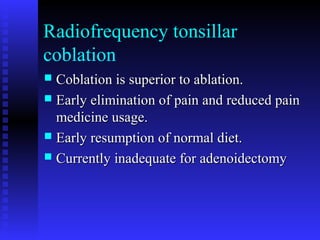
- Surgical indications and techniques for tonsillectomy and adenoidectomy
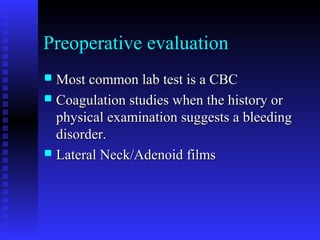
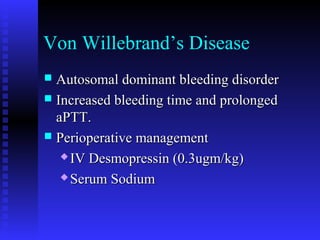
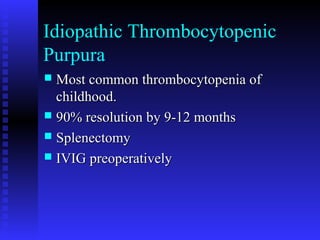
- Preoperative evaluation and management of bleeding disorders
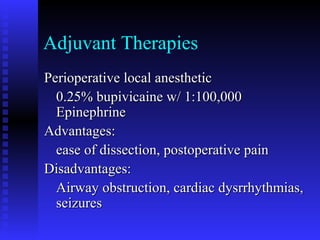
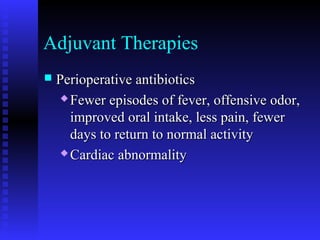
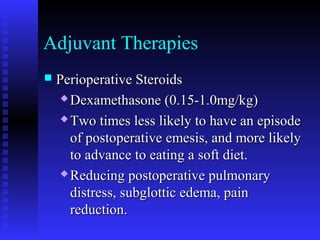
- Adjuvant therapies like antibiotics, steroids, and local anesthetics to improve postoperative outcomes