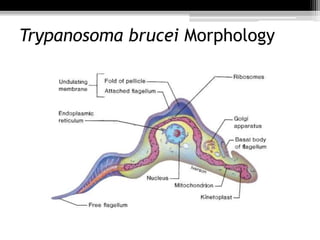
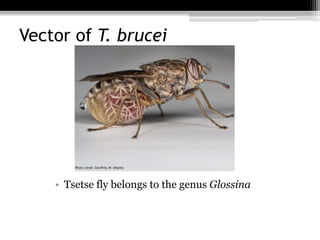
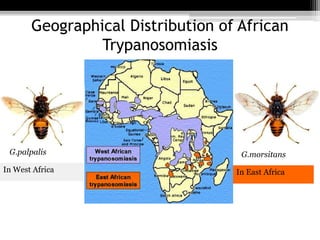
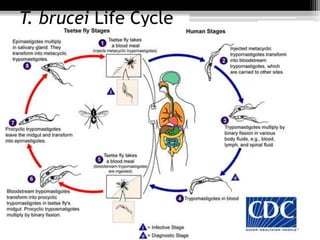
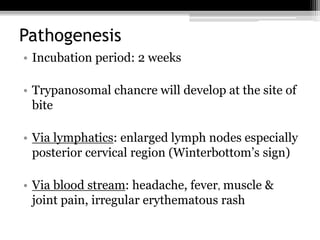
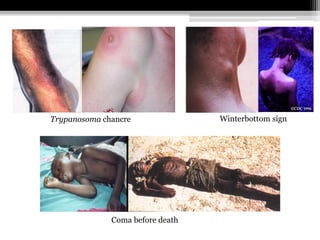
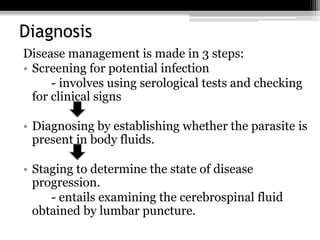
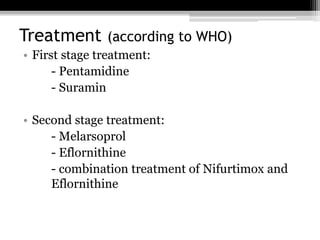
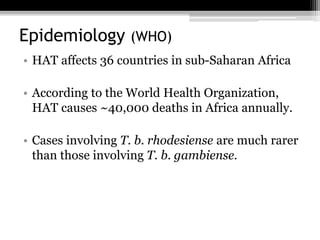
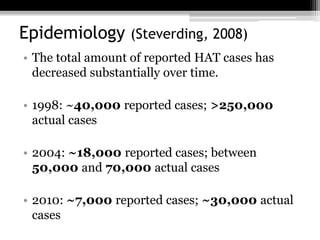
This document summarizes information about Trypanosoma brucei, the parasite that causes Human African Trypanosomiasis (HAT) or sleeping sickness. It describes the parasite's morphology, life cycle, subspecies that infect humans, vector, geographical distribution, stages of infection, pathogenesis, diagnosis, treatment, and epidemiology. HAT affects around 36 countries in sub-Saharan Africa and causes approximately 40,000 deaths per year, though reported cases have decreased significantly in recent decades.