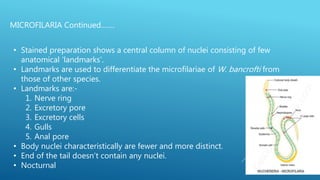
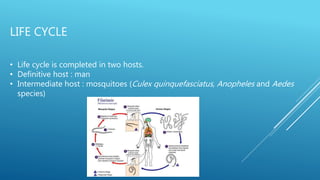
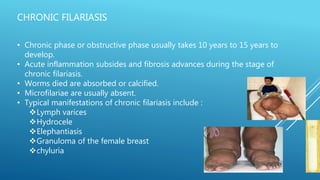
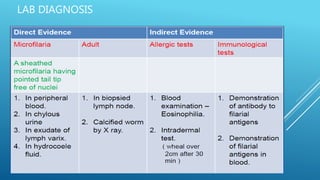
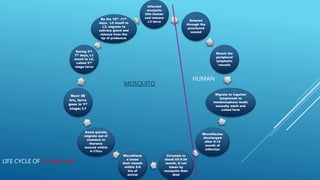
Wuchereria bancrofti is a filarial nematode parasite transmitted by mosquitoes that causes lymphatic filariasis in humans. The document outlines the life cycle and pathogenesis of W. bancrofti. It begins in the human host, passes through mosquito and human again. In humans, the adult worms reside in lymphatic vessels causing inflammation and dilation. Over time this leads to lymphedema and elephantiasis as lymphatic flow is obstructed. Diagnosis involves blood smears to detect microfilariae or provocative tests using diethylcarbamazine.