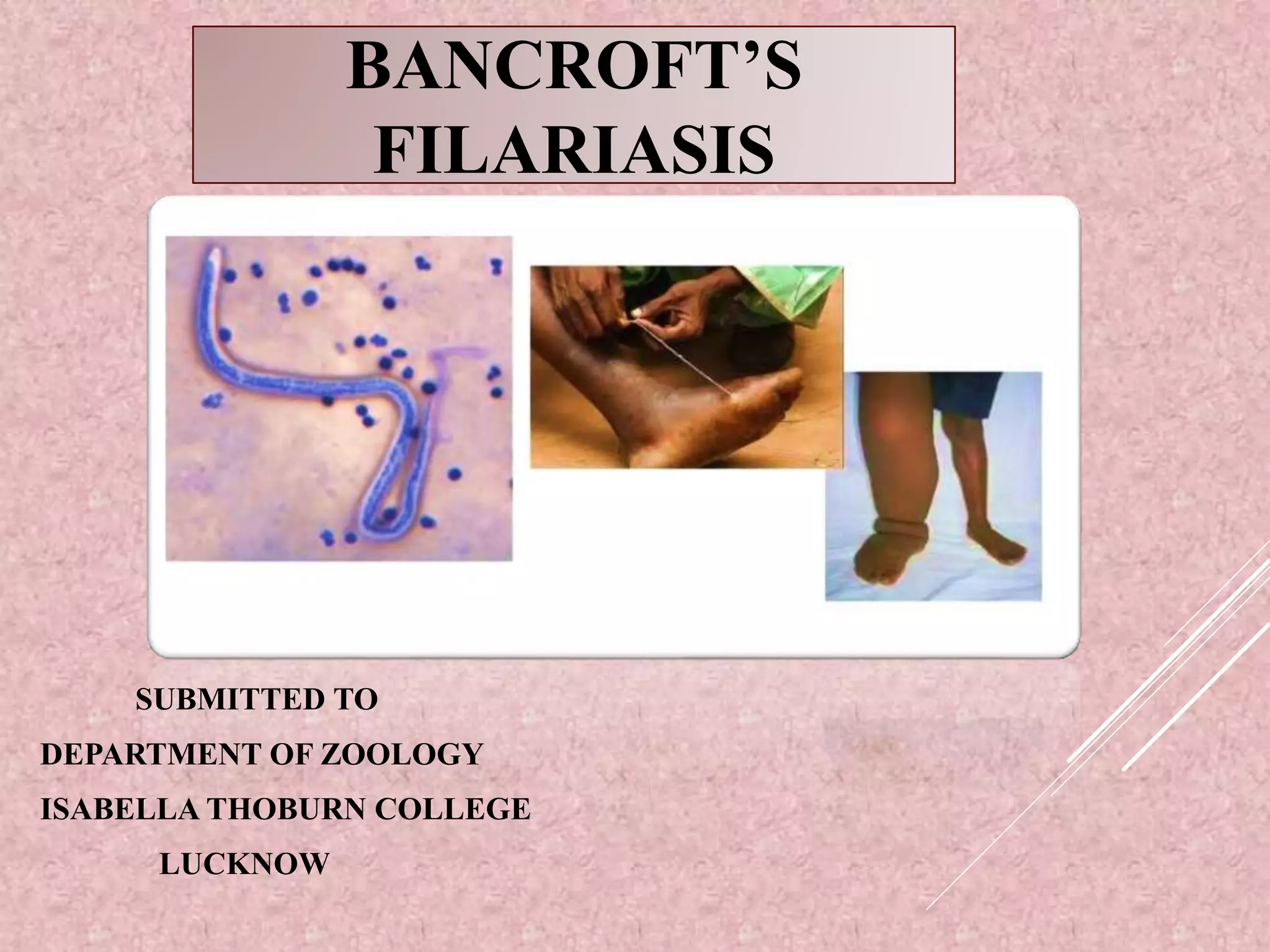
Wuchereria bancrofti is a parasitic nematode that causes lymphatic filariasis (elephantiasis) in humans. It is transmitted by mosquitoes and lives in the human lymphatic system. The parasite has a complex life cycle involving microfilariae in human blood that are ingested by mosquitoes during feeding. The mosquito serves as an intermediate host where the microfilariae develop into infective larvae, which are then transmitted to humans during subsequent blood feeding, developing into adult worms in the lymphatics. Clinical manifestations range from asymptomatic microfilaremia to lymphedema and elephantiasis of the legs and genitals due to long-term infection and damage.