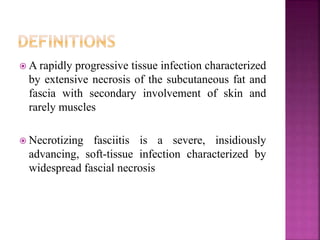
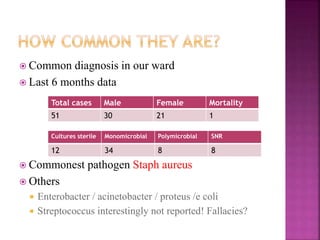
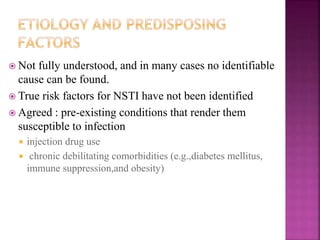
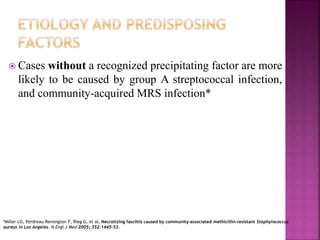
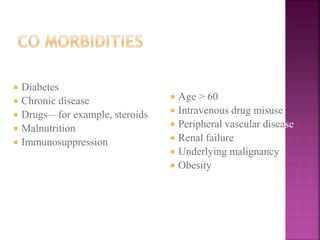
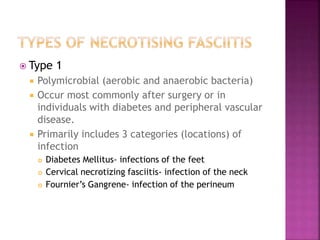
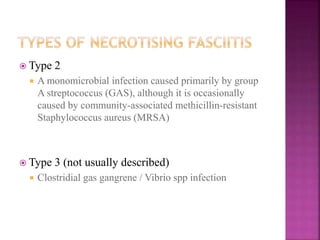
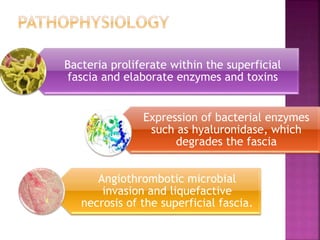
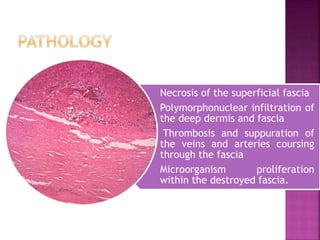
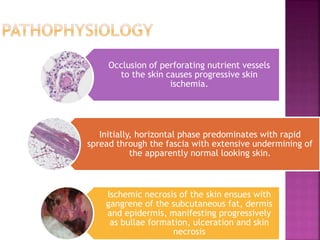
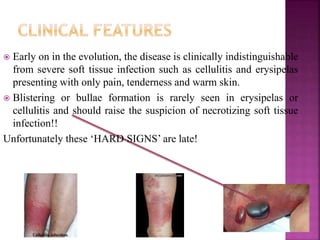
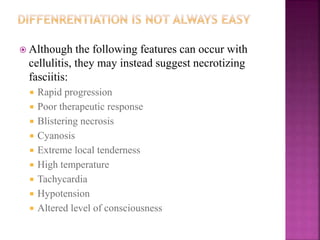
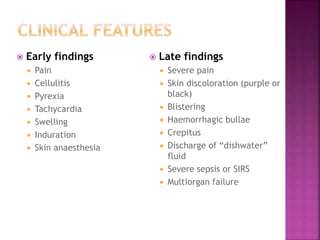
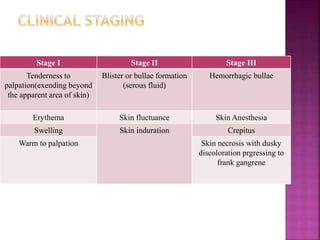
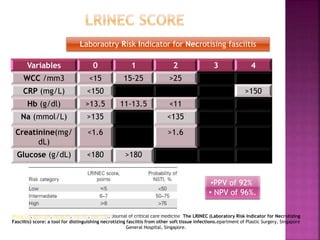
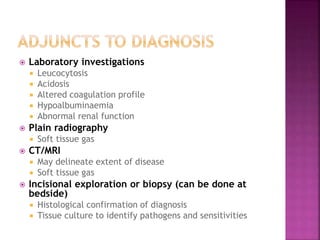
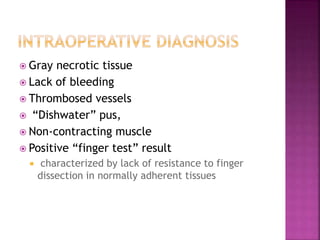
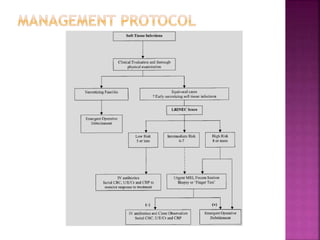
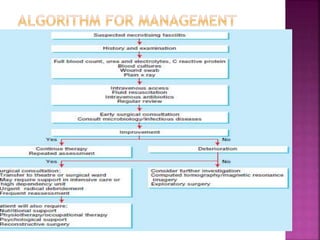
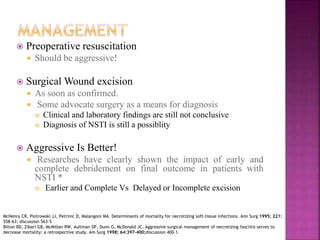
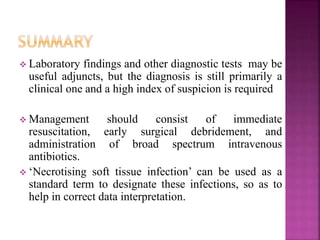
Necrotizing fasciitis is a severe, rapidly progressive soft-tissue infection characterized by widespread necrosis of the subcutaneous fat and fascia, often leading to high mortality rates due to delayed diagnosis. The condition affects individuals with pre-existing risk factors such as diabetes, immunosuppression, and invasive procedures, and presents with initial symptoms similar to cellulitis but requires immediate surgical intervention and aggressive management for better outcomes. Diagnosis is primarily clinical, relying on early symptom recognition and laboratory findings, with timely surgical debridement and broad-spectrum antibiotics being critical for survival.