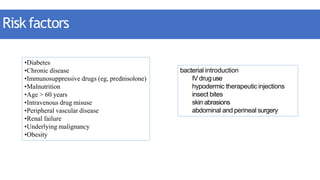
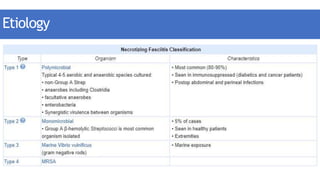
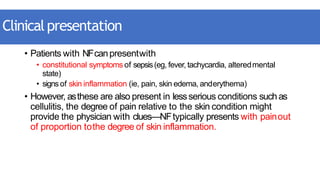
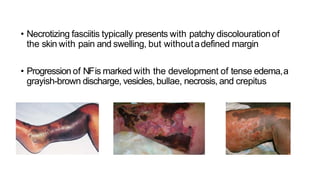
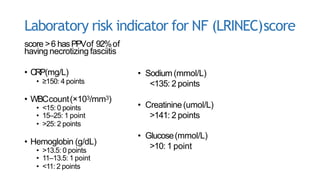
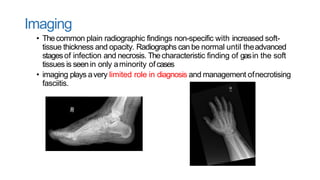
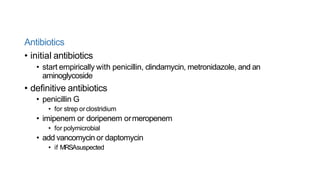
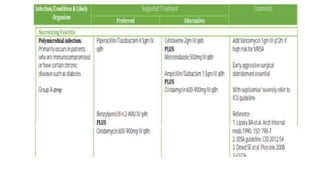
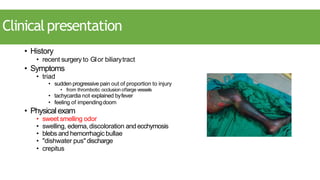
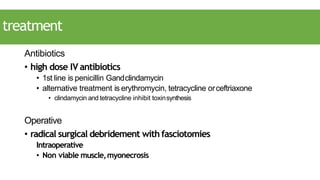
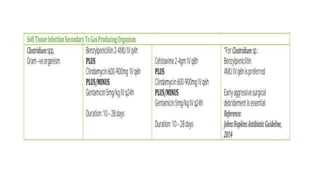
This document discusses necrotizing fasciitis and gas gangrene. It defines them as necrotizing soft tissue infections caused by bacteria. For necrotizing fasciitis, it lists risk factors like diabetes and clinical signs like disproportionate pain. Evaluation involves labs, cultures, and imaging. Treatment is emergent debridement and broad-spectrum antibiotics. Gas gangrene is caused by Clostridium bacteria following trauma. It presents with pain, swelling and a sweet odor, and is treated with surgery and antibiotics against Clostridium like penicillin and clindamycin.