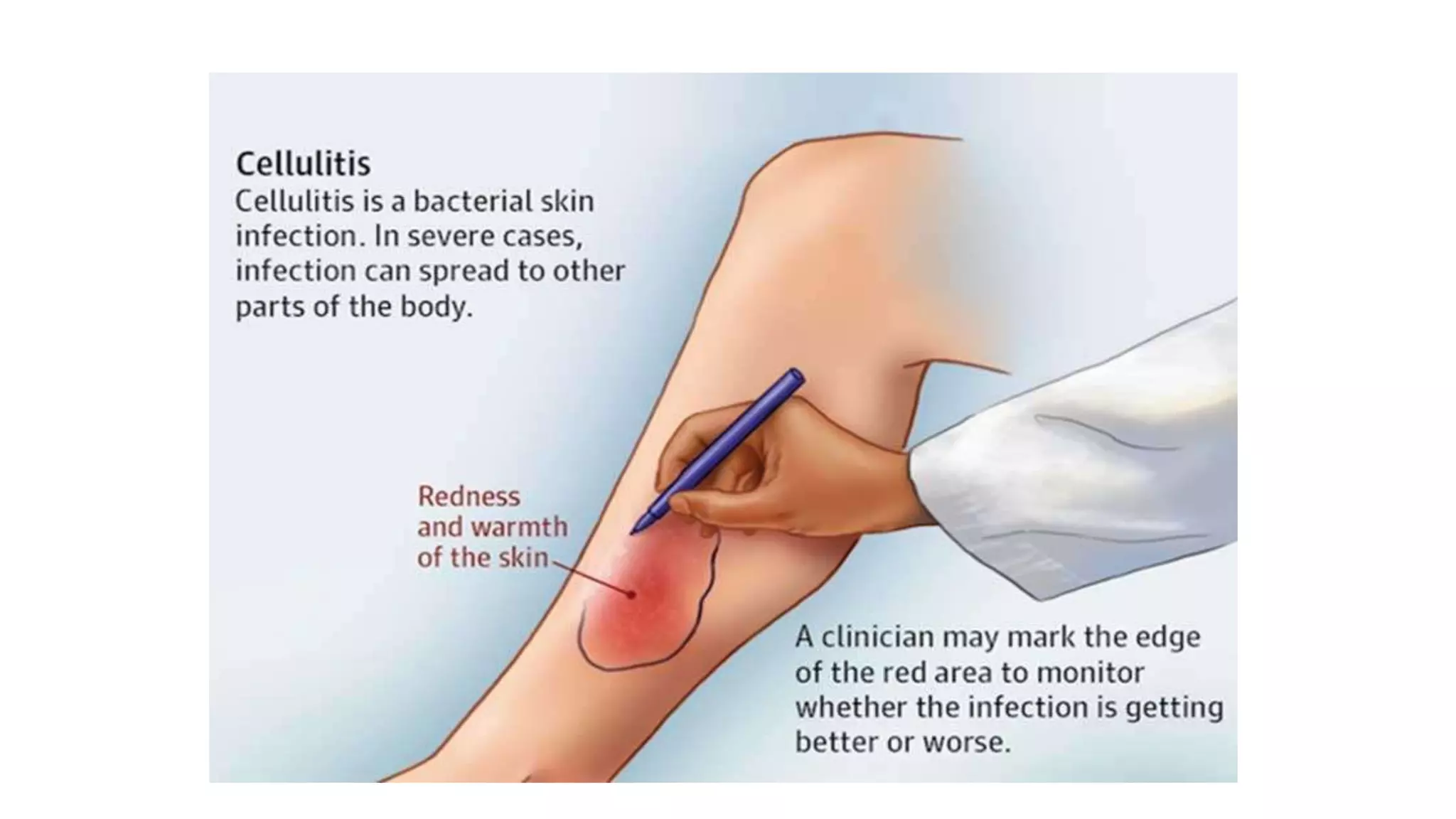
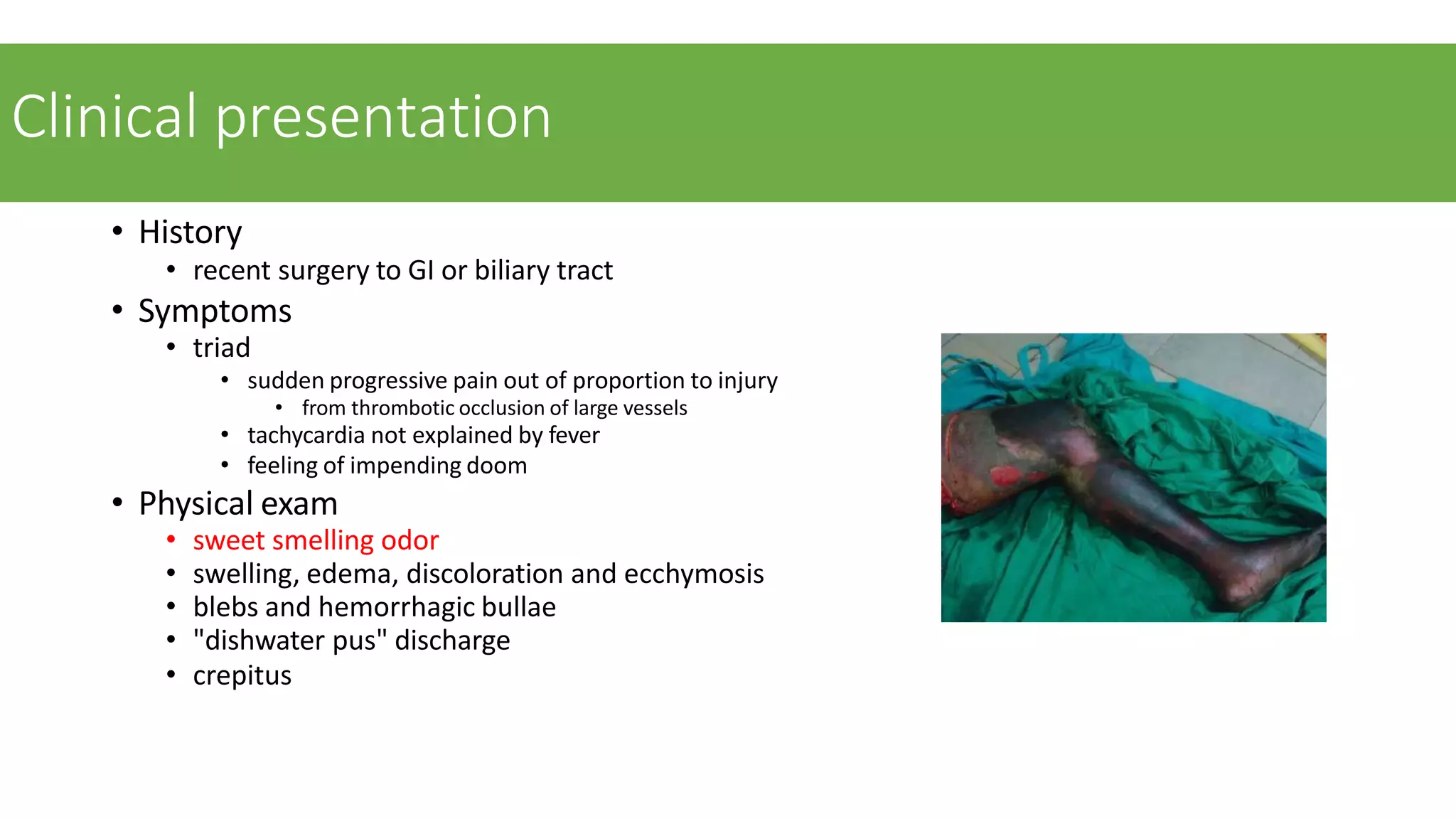
This document discusses cellulitis, necrotizing fasciitis, and gas gangrene. Cellulitis is a spreading skin infection below the skin surface caused commonly by Streptococcus bacteria. Necrotizing fasciitis is a serious soft tissue infection that spreads rapidly along fascial planes, and risk factors include diabetes and immunosuppression. Gas gangrene is a necrotizing soft tissue infection of muscle caused by Clostridium bacteria, often following trauma. It is characterized by pain, swelling, and crepitus or gas in tissues. Treatment for these conditions involves antibiotics, surgical debridement of infected tissues, and management of the underlying risk factors or injuries.