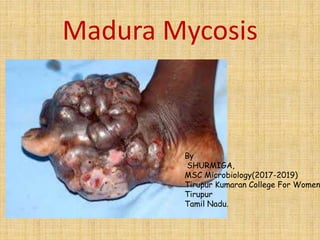
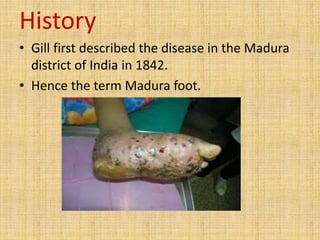
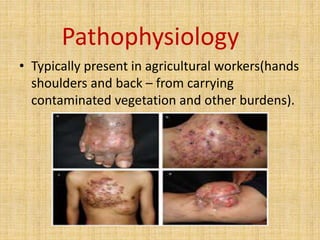
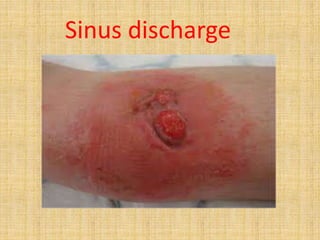
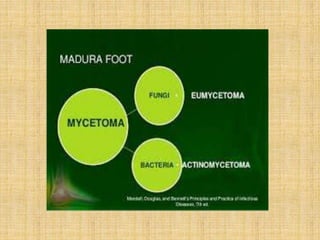
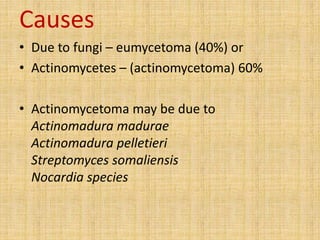
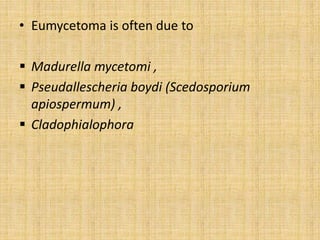
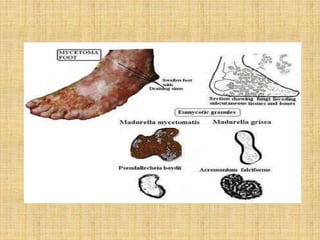
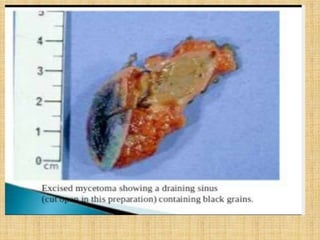
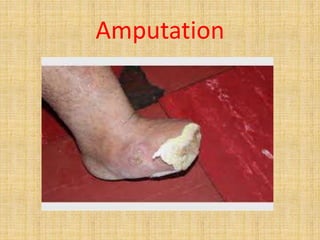
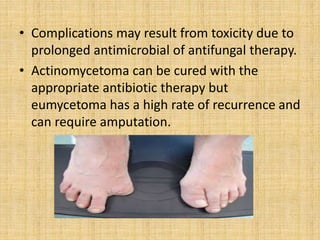
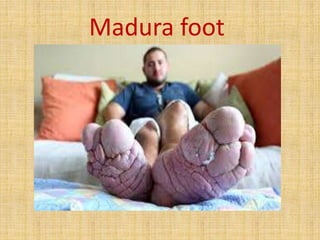
Madura mycosis, or mycetoma, is a chronic granulomatous disease characterized by localized infections that often affect the foot, typically seen in agricultural workers who are exposed to contaminated soil. The disease is caused by actinomycetes or fungi, leading to slow-progressing symptoms including swelling, pus discharge, and potential bone involvement. Treatment usually involves long-term antifungal or antibiotic therapy, and severe cases may require surgical intervention or amputation.