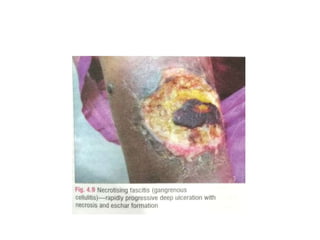
This document provides information about necrotizing fasciitis, also known as flesh-eating bacteria. It begins by defining necrotizing fasciitis as a rapidly spreading necrotizing infection of subcutaneous tissue and fascia. It then discusses the two main types, risk factors like diabetes and immunosuppression, pathophysiology where bacteria destroy tissue and impair the immune response, early clinical features like pain and swelling, advanced features like necrosis and eschar formation. It concludes by covering diagnostic tests, treatment which involves emergency debridement and IV antibiotics to prevent toxic shock syndrome and death.