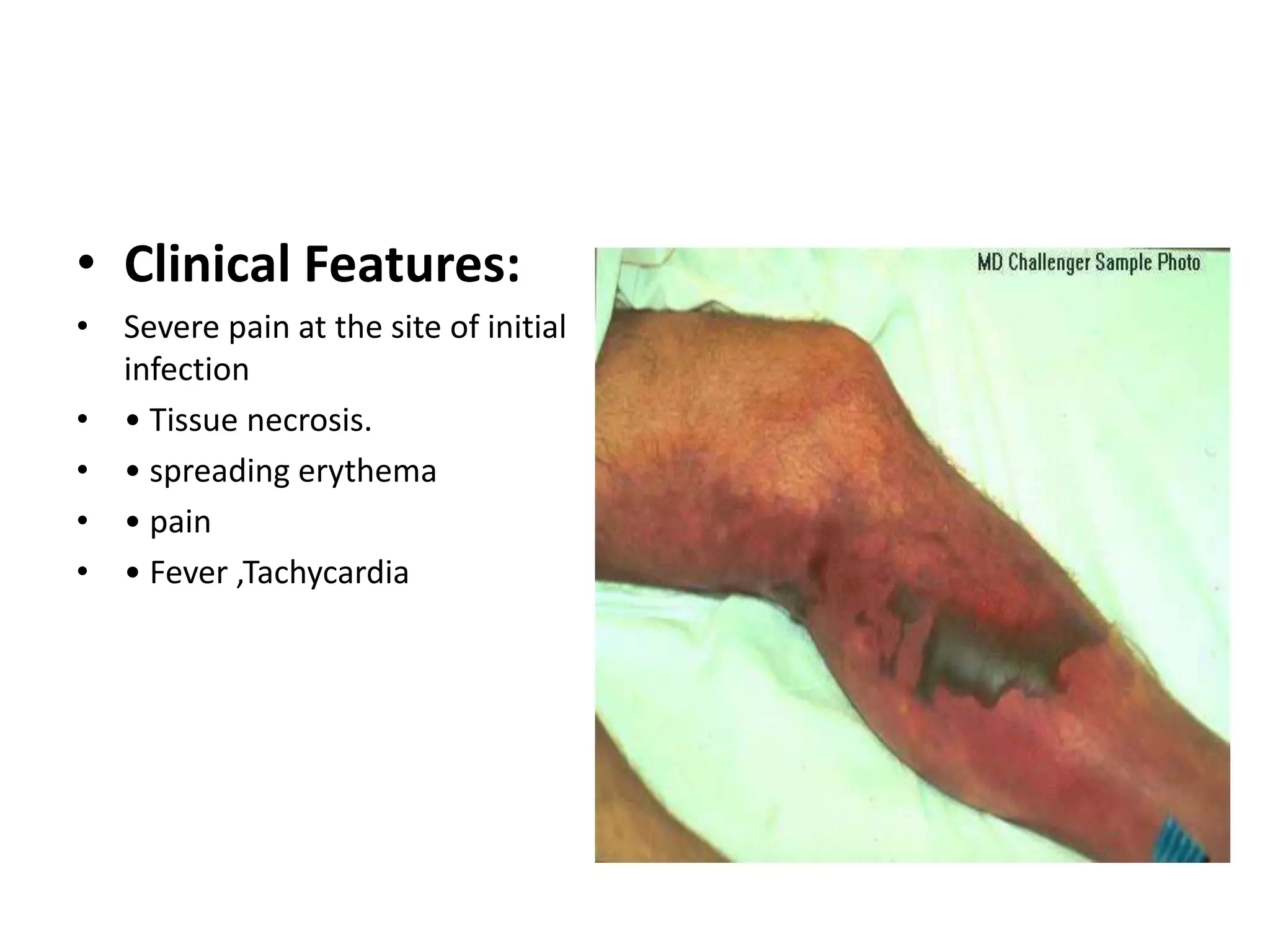
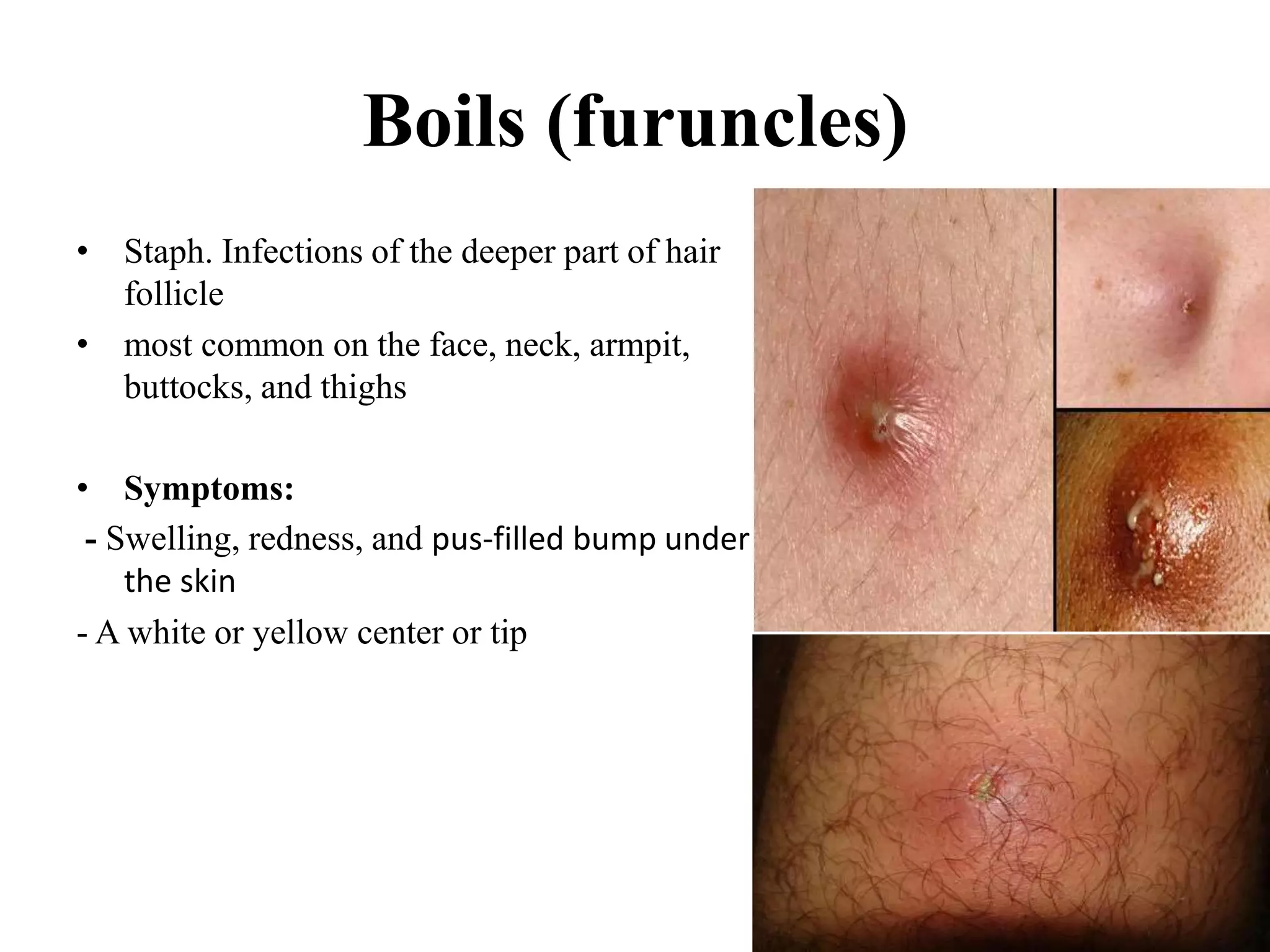
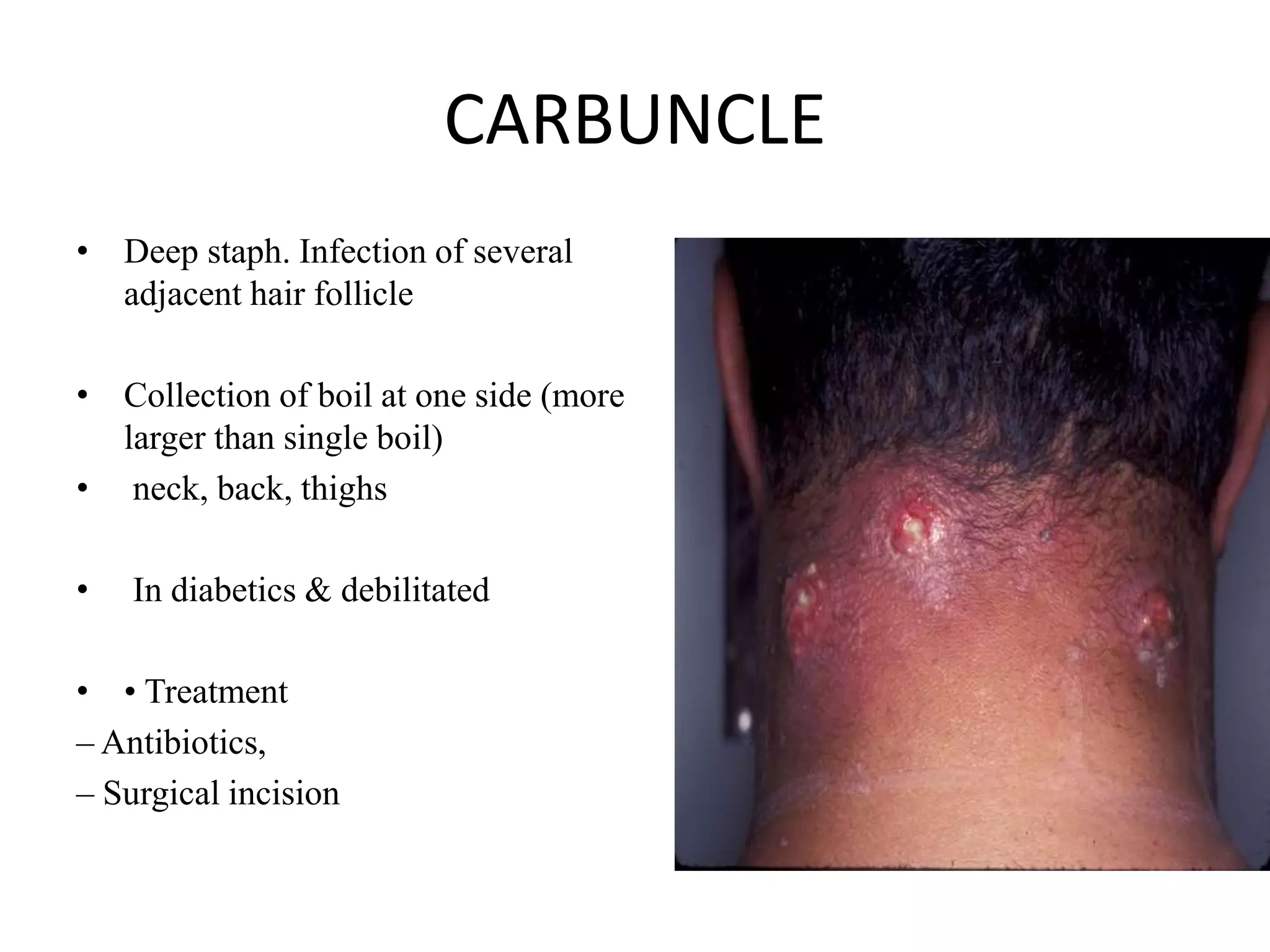
This document discusses various types of skin and soft tissue infections, including their causes, symptoms, and treatments. It covers primary infections like impetigo caused by streptococci or staphylococci and secondary infections like cellulitis. Deeper infections involving fascia and muscles are also outlined, such as necrotizing fasciitis caused by streptococci or clostridia. The diagnostic process involves specimen collection, microscopy, and bacterial culture and identification. Proper treatment depends on the identified pathogen and may involve antibiotics, surgery, or both.




















![• Classification : 4 types (types of bacteria infecting the soft tissue)
1) Type I infection: most common type (70-80 % cases) , abdominal or groin
areas ,
• Staphylococcus aureus, Streptococcus pyogenes, and enterococci ,
Escherichia coli, Pseudomonas aeruginosa, and anaerobes,
(Bacteroides and Clostridium species [ Clostridium perfringens, Clostridium
septicum, and Clostridium sordellii] )
• Trauma is not the cause of such infections ( Previous history of abscess
infection or gut perforation)](https://image.slidesharecdn.com/skinandsofttissueinfections-201204095940/75/Skin-and-soft-tissue-infections-26-2048.jpg)