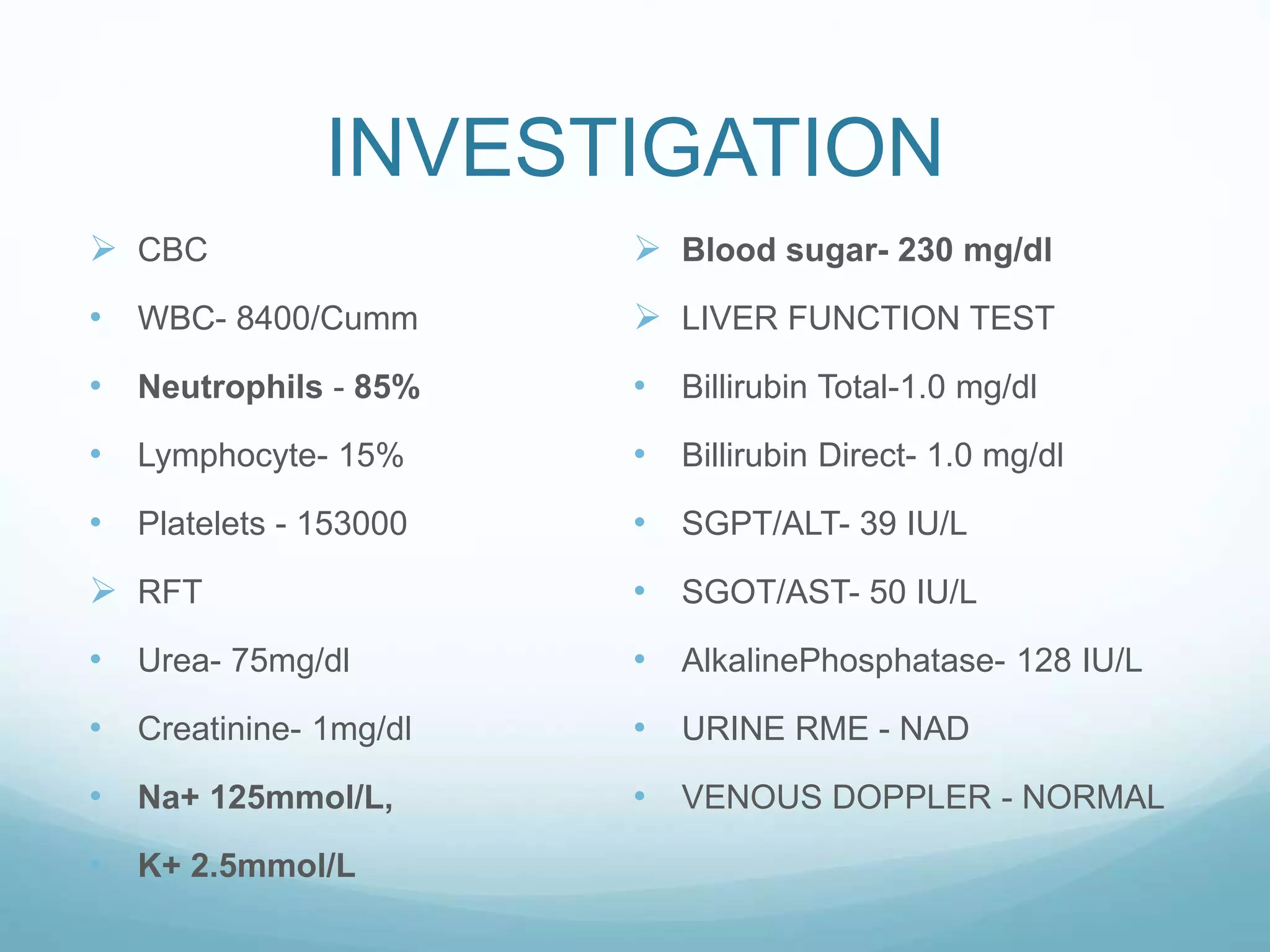
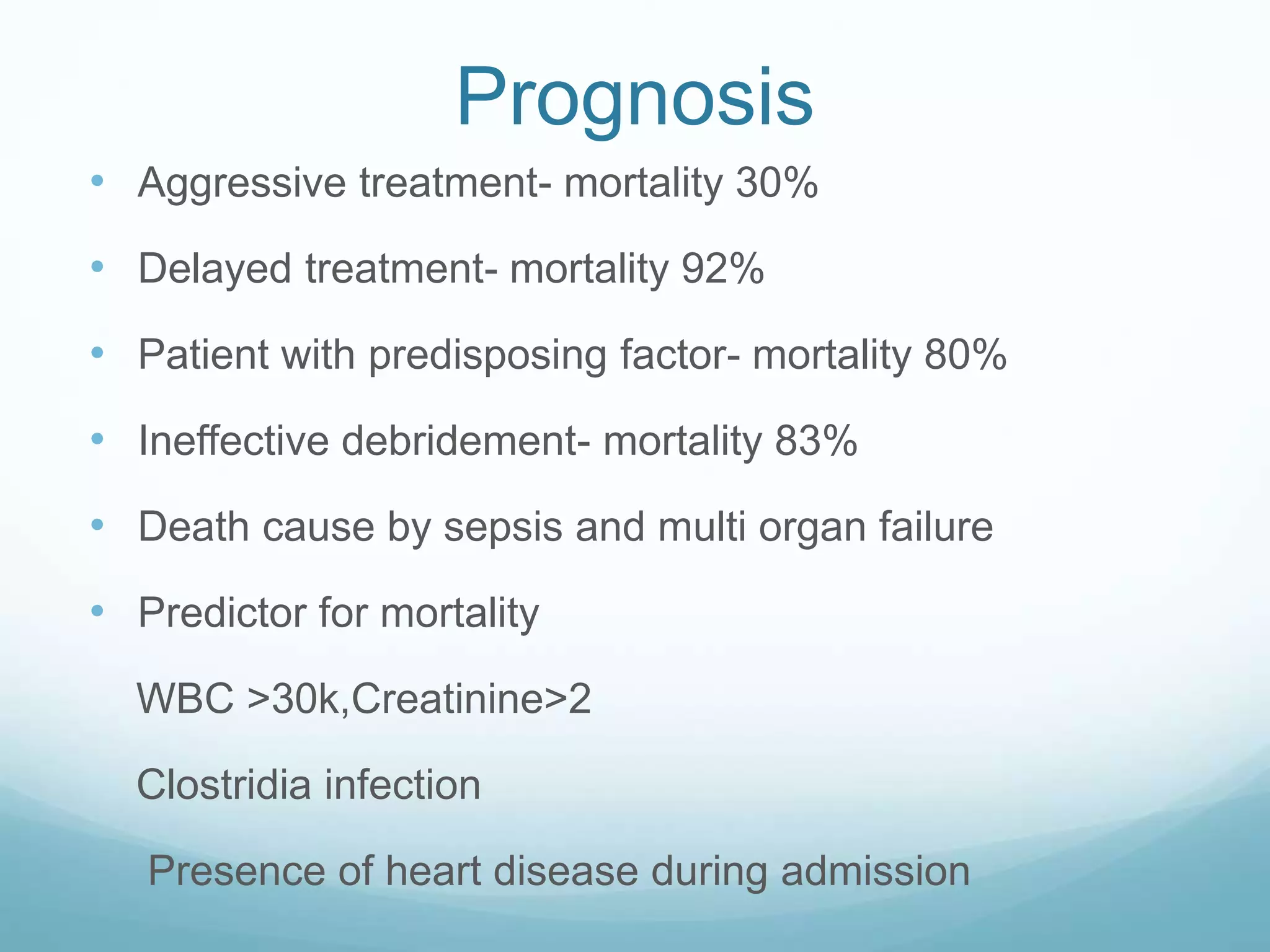
This document describes a case of necrotizing fasciitis in a 54-year-old man. The man presented with swelling and pain in his left lower leg, along with watery discharge and skin blisters. He had a history of an insect bite a month prior. Investigation revealed elevated white blood cell count and blood sugar. The patient was diagnosed with uncontrolled diabetes and necrotizing fasciitis. He underwent fasciotomy, debridement, and skin grafting. The wound culture grew Pseudomonas aeruginosa. With aggressive treatment including antibiotics, surgery, and control of his diabetes, the patient's condition improved.