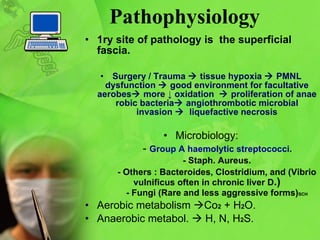
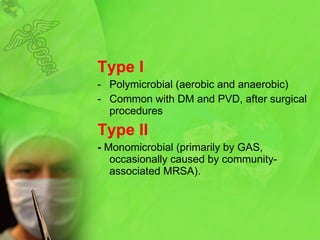
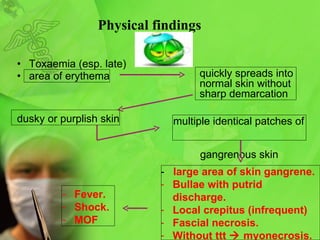
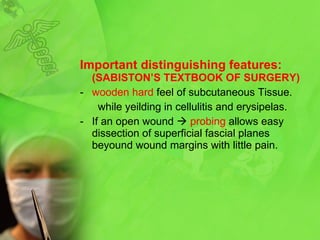
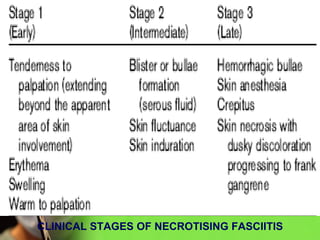
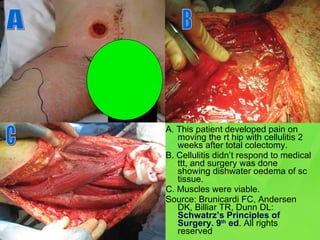
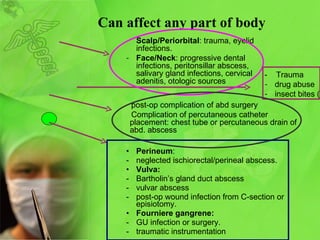
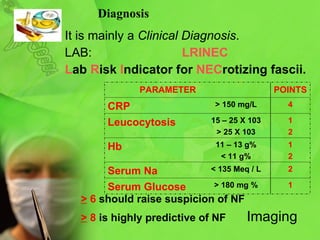
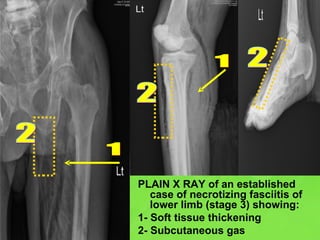
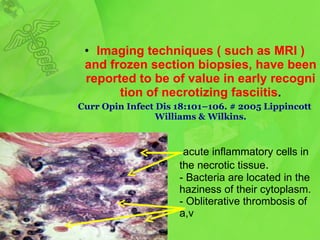
Necrotizing fasciitis is a life-threatening soft tissue infection characterized by necrosis of subcutaneous tissue and fascia. It is usually caused by bacteria entering through breaks in the skin or surgery. Clinically, it presents with severe pain and swelling spreading beyond the site of infection. Treatment requires aggressive antibiotic therapy and urgent surgical debridement of necrotic tissue to remove the infected areas. Despite treatment, complications can be severe and mortality remains high if not recognized and treated promptly.