VVF DR SR PATANAIK
- 1. Dr.SMRUTI RANJAN PATANAIK GUIDE – DR . NINA MISHRA
- 2. INTRODUCTION • A fistula represents an extra – anatomic communication between two or more body cavities covered by their own epithelia, the communicating tract is also epithelized. This tract may also open at the skin surface. • Classification of urinary fistulas is generally based on organ of origin in urinary tract and termination point of fistula.
- 3. TYPES OF GENITO URINARY FISTULAS BLADDER 1. VESICO VAGINAL 2. VESICO UTERINE 3. VESICO CERVICAL 4. VESICO URETHROVAGINAL URETER 1. URETERO VAGINAL 2. URETERO UTERINE 3. URETERO CERVICAL URETHRA 1. URETHRO VAGINAL
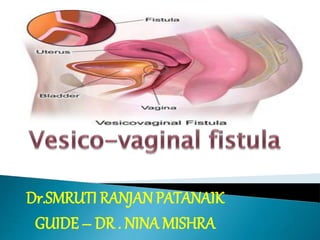
- 6. Vesico-vaginal fistula Vesicovaginal fistula (VVF) is an abnormal opening between the bladder and the vagina that results in continuous and unremitting urinary incontinence.. VESICO – VAGINAL FISTULA
- 7. HISTORY MOST COMMON ACQUIRED FISTULAS ANCIENT EGYPT, BEFORE 2000 BC DESCRIBED BY SIMS
- 8. CLASSIFICATION OF GENITOURINARY FISTULA ACCORDING TO FISTULA SITE, SIE, SCARRING AND VAGINAL LENGTH • SITE – 1. Type 1 : Distal edge of fistula > 3.5cm from external urinary meatus (EUM). 2. Type 2 : > 2.5cm – 3.5cm from EUM 3. Type 3 : > 1.5 cm – 2.5cm EUM 4. Type 4 : < 1.5cm from EUM
- 9. • SIZE – • Size < 1.5 cm in the largest diameter. • Size 1.5 cm – 3 cm in the largest diameter. • Size > 3cm in the largest diameter. CLASSIFICATION OF GENITOURINARY FISTULA ACCORDING TO FISTULA SITE, SIE, SCARRING AND VAGINAL LENGTH
- 10. • SCARRING AROUND AND VAGINAL LENGTH. 1. None or mild fibrosis around fistula and / vaginal length > 6cm. 2. Moderate or severe fibrosis around fistula and reduced vaginal length. 3. Special cases e.g. Post radiation, ureteric involvement, previous repair. CLASSIFICATION OF GENITOURINARY FISTULA ACCORDING TO FISTULA SITE, SIE, SCARRING AND VAGINAL LENGTH
- 11. Classification according to site of fistula CLASSIFICATION ACCORDING TO SITE OF FISTULA 1. HIGH FISTULA – JUXTA CERVICAL VAULT (VESICO – UTERINE) 2. MID VAGINAL FISTULA 3. LOW FISTULA – BLADDER NECK (URETHRA INTACT) URETHRAL INVOLVEMENTS ( SEGMENTAL, i.e Partial Bladder Neck Loss ) COMPLETE BLADDER NECK LOSS (CIRCUMFERENTIAL FISTULA) 4. MASSIVE VAGINAL FISTULA Encompasses all three fistulas and may include one/both ureters in addition.
- 12. CLASSIFICATION ACCORDING TO SIZE • SMALL -- < 2Cms • MEDIUM – 2 – 3 Cms • LARGE – 4 – 5 Cms • EXTENSIVE -- > 6 Cms
- 13. CLASSIFICATION ACCORDING TO COMPLEXITIES SIMPLE VVF • < 2 – 3 cms in size. • Supra Trigonal • No H/O of pelvic malignancy and radiation. • Vaginal Length is normal. • Healthy Tissue • Good Access COMPLEX VVF • > 3 cms in size. • Trigonal or Below • H/o – Pelvic Malignancy or radiation • Vaginal length is shortened • Associated with scarring • Involving Urethra, Vesical Neck, Ureter • Previous unsuccessful attempt at repair.
- 15. ECTOPIA VESICAE (CONGENITAL) • The posterior wall of the urinary bladder is exposed to the exterior. • It is caused by the failure of the anterior abdominal wall and anterior wall of the bladder to develop. • It is due to inability of the mesoderm of the primitive streak to migrate around the cloacal membrane. • Aberrant Ureter and persisting uro genital sinus.
- 17. ETIOLOGY • OBSTETRICAL TRAUMA ( 95 %) - Prolonged and obstructed labour---pressure necrosis of bladder neck or trig one leads to delayed onset of urinary fistula during second week of puerperal due to constant and prolonged compression of bladder neck by jammed up presenting part against symphysis pubis as in cases of obstructed and prolonged labour . - Till mid 6th decade of last century; this was the commonest cause of obstetrical urinary fistula . change in the management of CPD , contracted pelvis , malpresentation ,Uterine inertia has made it a remote complication. - Introital stenosis secondary to female circumcision , cephalopelvic disproportion, an android pelvis , malnutrition , orthopaedic disorder contribute to dystocia . - operative(iatrogenic)--- forceps (kielland’s /high forceps application ,destructive instruments used to deliver stillborn infants and criminal abortion. Gishiri cuts(nigra)
- 19. POST SURGICAL - - - - GYNAECOLOGICAL-----(0.5 -1 %) Abdominal hysterectomy(1/1300patients)Simple / redical(Werthem’s.) Vaginal hysterectomy. Myomectomy—cervical and broad ligament fibroids. Laparoscpic --- fulguration, too much heat near bladder or ureter - Caesarean section - Sling operation for-incontinence of urine. - Repair of Anterior vaginal wall prolapse -- (e.g.colporrhaphy) - Manchester Repair. - Circlage operation with separation of bladder at the level of internal Os. Vaginal cystectomy. Cystoscopic---Bladder biopsy , Endoscopic resection , laser procedure
- 20. • Radiation induced fistula (associated with Rx for Cancer Cervix or other pelvic malignancies) • Vaginal foreign bodies • Forgotten Pessaries • Direct trauma from masturbation or automobile accidents • Miscellaneous- Late stage of malignancy of genital tract involving urinary tract. • Tuberculosis , Schistosomiasis , Perforating bladder calculi , Endometriosis , Syphilis , Lymphogrannuloma venerum and idiopathic and congenital cause. OTHER CAUSES
- 21. CLINICAL FEATURES • VVF usually presents with constant/continuous leakage of urine per vagina (True Incontinence) – Classic Symptom. • Leakage after surgical injury occurs from the first post operative day. • Most commonly recognized in first 10 days after operation and less commonly between 10th to 20th postoperative day. • Obstetric Fistulas– Symptoms take 7-14 days to develop. • Post Pelvic Radiations Fistulas– Delayed Onset of Leakage, takes months to years. • Small Fistulas– Leakage in certain positions and can also pass urine normally. • Large Fistulas– Patientmay not void at all, but leak.
- 22. • Excoriation of Skin leads to fungal infection , irritation , dermatitis. • Recurrent cystitis or UTI. • Unexplained fever ,hematuria ; discomfort in flank and suprapubic region • As urea is split by vaginal flora, the vaginal pH becomes alkaline, which precipitates greenish-gray phosphate crystals in the vagina and on the vulva. • The patient can become a social recluse; disrupt sexual relations; and lead to depression, low self-esteem, and insomnia. CLINICAL FEATURES
- 23. HISTORY • Age and socioeconomic status of the women. • Previous gynecological surgery/radiotherapy. • Previous h/o prolonged labour/trauma during child birth. • Time of occurence. • History of Urine Leakage. • Timing of leakage, amount of leakage. • Voiding per urethra apart from leakage. • Any leakage of feces, gas leakage. • Any attempt of previous repair of fistula.
- 24. PHYSICAL EXAMINATION • General Examination • Per abdomen examination – surgical scars Vulval Inspection -- Leakage of urine and excoriation of vulva, escape of watery discharge per vaginum of ammoniacal smell is characteristic, sudden and excoriation of the vulval skin, varying degree of perineal tears may be present.
- 25. • P/S Examination – • Sim s speculum and sim s position • Pool of urine in vagina and fistulous opening may be visible. • Location, number and size of fistula is to be noted. • In case of bladder neck fistula involvement of internal sphincter may also be associated . • There may be associated or combined fistulas e-g vesico vaginal , vesicocervical and ureteric fistula. Bladder mucosa may be visibly prolapsed through a big fistula
- 27. DIAGNOSIS • SPECIAL TESTS – 1. CATHETER TEST – comes out from the vaginal orifice of vagina. 2. CLICK TEST – metal catheter in bladder gives click with metal probe passes through vaginal orifice of fistula. 3. METHYLENE BLUE DYE TEST 4. MODIFIED METHYLENE BLUE TEST– no pads but dye is observed directly. 5. DOUBLE DYE TEST ---
- 28. DYE TEST TO DETECT THREE SWAB TEST To, differentiate from ureterovaginal and urethrovaginal INTRAVENOUS UROGRAPHY Ureterovaginal fistula RETROGRADE PYELOGRAPHY Exact site of Ureterovaginal fistula CYSTOGRAPHY Vesiciouterine fistula SINOGRAPHY (FISTULOGRAPHY) Intestinogenital fistula HYSTEROSALPINGOGRAPH Y Vesicouterine fistula USG, CT, MRI Complex fistula CYSTOURETHROSCOPY Location of fistula in relation to ureteric orifice
- 29. DYE INSTILLATION • Although the ideal method of confirming genitourinary fistulas is by direct visualization, there are instances where physical examination and inspection are unrevealing these circumstances, bladder instillation of visually distinct solutions such as methylene blue, sterile milk and indigo carmine can often indicate the location.
- 30. • When the presence of a urinary fistula is uncertain, or the location in the vagina cannot be identified, a modified tampon test or three swab test is recommended. • During testing, gauze is packed sequentially into the vaginal canal. A diluted solution of Indigo Carmine/Methylene blue is instilled into the bladder in a retrograde fashion, using a catheter. • After the patient has engaged in 15 – 30 minutes of routine activity, the gauze is removed serially from the vagina and inspected for the presence of dye. • The specific gauze coloured with dye suggests, where in the vagina a fistulous tract is located – a proximal or high location in the vagina for the innermost gauze, and low or distal fistula for the outermost. • If the distally placed gauze is stained with dye, however, it is important to confirm that it was not contaminated by stress incontinence
- 34. INVESTIGATIONS • CBC and Urine analysis • Blood chemistry for serum creatinine , blood urea and fasting blood sugar. • Urine for culture and sensitivity. • Intravenous pyelography (Ureteric fistula ,ureteric stricture and hydronephrotic changes) • Ascending pyelography to fortify the findings of IVP. • Modern imaging technique CT and MRI have limited value as Cystoscopy ( performed)gives maximum and to the point information about size ,shape , number and location of fistulas. • Biopsy from the edge of fistula cystoscope guided when it is suspected to be – malignant/post radiation/tubercular /schistosomiasis
- 42. PREVENTION • OBSTETRIC FISTULA PRIMORDIAL PREVENTION 1. Girl’s Education 2. Women’s Empowerment 3. Increase the age of marriage 4. Nutritious diet since childhood
- 43. PREVENTION • PRIMARY PREVENTION 1. Availability of family planning method services. 2. Strategy to make motherhood safer should be followed. 3. Good antenatal care. 4. Watchful progress of labour. 5. Trained birth attendants. 6. Transportation of emergency obstetric care.
- 44. PREVENTION • SECONDARY PREVENTION 1. Early recognition of CPD and prevention of obstructed labour. 2. LSCS in indicated cases. 3. Avoidance of difficult forceps and destructive operations 4. Prolonged catheter drainage in prolonged obstructed labour.
- 45. PREVENTION • RADIATION FISTULA 1. Proper dose and technique of irradiation 2. Packing of the vagina 3. Midline Block
- 46. IF WE SUSPECT FISTULA IS GOING TO FORM AFTER OBSTRUCTED LABOUR OR DESTRUCTIVE OPERATION • Insert an indwelling catheter and start continuous closed drainage. • Ensure a high fluid intake. • Mobilise her early, always keeping the bag below her bladder. • After 7- 10 days , examine her anterior vaginal wall in Sim’s position with speculum. • If her bladder is still bruised or necrotic, then leave her catheter in and remove only when healthy tissue is seen in next examinations.
- 47. PREVENTION • SURGICAL FISTULA 1. Adequate exposure during surgery. 2. Minimize bleeding and hematoma formation 3. Dissection in correct planes. 4. Wide mobilisation of the bladder. 5. Intra op retrograde filling of bladder. 6. Cystourethroscopy during surgery.
- 48. MANAGEMENT 1.CONSERVATIVE MANAGEMENT 2.MEDICAL THERAPY/INTERVENTION 3. NON SURGICAL INTERVENTION 4.SURGICAL THERAPY/INTERVENTION
- 49. CONSERVATIVE MANAGEMENT • INDICATIONS 1. Simple fistulae 2. < 1cm in size 3. Diagnosed within 7 days of index surgery. 4. Unrelated to carcinoma or radiation. CONTINUOUS BLADDER DRAINAGE 1. By transurethral or supra pubic catheter. 2. Duration upto 30 days Small fistula may resolve spontaneously, if fistula decrease in size then drainage for additional 2-3 weeks If no improvement in 30 days then will need surgery.
- 50. MEDICAL THERAPY/INTERVENTION • Estrogen Replacement Therapy – optimise tissue vascularization and healing in post menopausal patient. • Local Estrogen Vaginal Cream – 2-4 grams placed per vaginally at bedtime once a week for 4-6 weeks in those who are hypo estrogenic. • Acidification of Urine– to diminish risk of cystitis, bladder calculi formation, vitamin C 500mg orally TDS
- 51. • Antibiotics – to prevent infection of the site. • Other Drugs – Combination of antiseptics like methenamine, phenyl salicylate, methylene blue, benzoic acid. Parasympatholytics like atropine sulphate , hyoscyamine sulphate. Sitz Bath Barrier ointment such as zinc oxide or vaseline application In treatment of perineal and ammoniacal dermatitis. MEDICAL THERAPY/INTERVENTION
- 52. NON SURGICAL INTERVENTION/THERAPY • ELECTROCAUTERY FULGURATION – Fistula small in size (pin hole openings) Vaginal and cystoscopic route – fulguration – foley’s catheter placement for 2-3 weeks. FIBRIN GLUE – useful and safe for intractable fistula LASER WIELDING WITH ND YAG LASER – Fulguration and transurethral catheter for 3 weeks.
- 55. SURGICAL MANAGEMENT • PRINCIPLES 1. Timing of Repair 2. Route of Repair 3. Suitable equipment and illumination 4. Adequate exposure and patient positioning 5. Excision of fistulous tract 6. Use of suitable suture material 7. Sufficient post operative bladder drainage.
- 56. TIMING OF REPAIR • Dictum is that , the best time to repair fistula is at its first closure during index surgery. • Obstetric Fistula – 3 months following delivery • Surgical Fistula – if recognised within 48 hours or immediate repair. Otherwise repaired after 10 – 12 weeks. • Radiation Fistula – after 12 months.
- 57. PREOPERATIVE CARE • Improvement of general conditions • Continuous bladder drainage • Antibiotics • Estrogen cream • Topical creams for ammoniacal dermatitis
- 59. PREOPERATIVE ASSESSMENT • Local assessment of the fistula best done 1 – 3 days before the repair – fistula status. • Urine Routine Microscopy • Urine Culture and Sensitivity • Cystoscopy • Urethroscopy • Voiding Cystourethrogram • Intravenous urogram • Retrograde Pyelogram • Urodynamic Studies DEPENDING ON CAUSE
- 63. PRINCIPLE OF FISTULA REPAIR • Adequate exposure of fistula tract with debridement of devitalised and ischaemic tissues . • Removal of involved foreign bodies or synthetic materials from region of fistula(if possible). • Careful dissection and anatomic separation of the involved organ cavities. • Water tight closure. • Use of well vascularized ,healthy tissues flaps of repair(traumatic handling of tissue). • Multiple layer closure. • Tension free, non-overlapping suture lines
- 64. Vaginal approach, Vaginal Flap splitting Latzko technique Saucerization Transvesical •Vertical cystotomy •Excision of VVF track transvesically Transperitoneal Combined VAGINAL APPROACH ABDOMINAL APPROACH SURGICAL MANAGEMENT
- 65. PEDICAL INTERPOSITION GRAFTS • For repair of big fistula, post radiation fistula AIM – •To support fistula repair •To fill dead space •To bring in new blood supply to area ofrepair. GRAFTS – •Martius graft-labial fats and bulbocavernousmuscle •Gracilis •Omental graft •Rectus abdominis •Peritoneal flap graft
- 66. ABDOMINAL APPROACH INDICATIONS • High inacessible fistula • Multiple fistula • Involvement of uterus or bowel • Need for ureter re-implantation • Complex fistula • Associated pelvic pathology • Surgeon preference
- 67. VAGINAL APPROACH ADVANTAGES • Avoids laparotomy and splitting of the bladder. • Recovery is shorter with less morbidity. • Less blood loss and postoperative bladder irritability. • Postoperative pain is minimal. • Results as successful as those of the abdominal approach are. • Vaginal shortening may be an issue with some types of vaginal vvf repairs, including the latzko operation.
- 68. ABDOMINAL APPROACH ADVANTAGES 1.Inadequate exposure related to a high or retracted fistula in a narrow vagina. 2.Close proximity of the fistulous tract to the ureter. 3.Associated pelvic pathology requiring simultaneous abdominal surgery. 4.Multiple and recurrent fistulas. 5.Supratrigonal location. 6.Surgeon's inexperience with vaginal surgery. 7.Tension free suturing. 8.Mobilization of bladder and excision of scar tissue. 9.Closure in layers. 10. Interposition of grafts particularly omentum and muscle. 11.Good exposure and spot less bright light. 12.surgeons experience with best route as well as location/size/number/associated uretericfistula.
- 74. A: A longitudinal incision is placed in the bladder dome. B: The incision is extended around the fistula. The fistulous tract and its vaginal orifice are completely excised. C: Interrupted delayed-absorbable sutures are used to close the vagina in one or two layers.
- 75. D: Continuous delayed-absorbable suture closes the bladder mucosa longitudinally. E: A suprapubic catheter is placed into the bladder in an extra peritoneal location.
- 76. F: The bladder muscularis is closed with delayed-absorbable continuous or interrupted sutures. G: An omental flap can be interposed between the bladder closure and the vaginal closure.
- 80. A: Ureters have been catheterized. An incision through the vaginal epithelium is made circumferentially around the fistula. B: The vaginal epithelium is widely mobilized from the bladder. The scarred fistula tract should be excised.
- 81. C: A continuous (or interrupted) delayed-absorbable suture inverts the mucosa into the bladder. D: A second suture line is placed in the musculofascial layer to reinforce the first. Vaginal epithelium is trimmed and approximated
- 82. Latzko technique for a closure of a simple vesicovaginal fistula. (A)A circumferential incision is made around the fistula. The fistula is not excised. B: The vaginal epithelium is mobilized approximately 2 cm from the fistula.
- 83. C: Delayed-absorbable interrupted mattress sutures are placed parallel to the edge of the fistula tract to invert it into the bladder. D: One or two additional rows of suture approximate the musculofascial layer of the bladder.
- 84. The vaginal epithelium is closed transversely with interrupted delayed-absorbable sutures.
- 85. A: The lateral margin of the labia majora is incised vertically) The fat pad adjacent to the bulbocavernosus muscle is mobilized, leaving a broad pedicle attached at the inferior pole.
- 86. C: The fat pad is drawn through a tunnel beneath the labia minor and vaginal mucosa and sutured with delayed-absorbable sutures to the fascia of the urethra and bladder. D: The vaginal mucosa is mobilized widely to permit closure over the pedicle without tension. The vulvar incision is closed with interrupted delayed-absorbable sutures.
- 87. ADVANCED SURGICAL TECHNIQUES • LAPAROSCOPY – Done mostly through the transvesical procedure. • ROBOTIC SURGERY – Complex and multiple fistula , or patients having dense adhesions.
- 88. POST OPERATIVE CARE • The bladder should be drained for 14 – 21 days. • Excellent hydration to ensure irrigation of the bladder and to prevent clots that could obstruct the bladder. • Catheter blockage should be prevented so that there is no bladder distension and tension on the suture lines. • Supra pubic catheter may be used for fistula in bladder. • Cystogram is to evaluate the integrity of the bladder before discontinuing the bladder drainage.
- 89. INSTRUCTION ON DISCHARGE • Contraceptive advice, i.e.Spacing for 1- 2years. • Abstinence for 3 months. • Maintain hygiene. • If pregnancy occurs elective C section is indicated at when fetus attains maturity. • Woman who had repair of obstetrical fistula may develop UTIs , DUB and other gynaecologyical problems like other people, should go for medical advice. • When pelvic surgery is indicated should be done by experienced surgeons.
- 90. FOLLOW UP • 2-3 Weeks after fistula repair is an adequate time period for post operative imaging. • At 6 weeks and 12 weeks clinical examination is to be done.
- 91. FACTORS AFFECTING SUCCESSFUL OUTCOMES • Adequate exposure of the operative field should be obtained to avoid inadvertent organ injury and to ensure early identification of any injury occurred.. • Minimize bleeding and hematoma formation. • Widely mobilize the bladder from the vagina to diminish the risk of suture placement into the bladder wall. • Adequate urinary tract drainage and catheterization. • Treatment and prevention of infection (Appropriate use of antimicrobials). • Wide mobilization of the vaginal epithelium to expose the bladder
- 92. POST OPERATIVE COMPLICATIONS EARLY 1. Excessive Bleeding 2. Surgical Wound infection 3. Urinary tract infection 4. Continued urine leakage through fistula LATE 1. Risks of abdominal and pelvic adhesions (if abdominal approach is used) 2. Risks of dyspareunia and tenderness (if vaginal approach is used) 3. Reduced vaginal length/ shortening and stenosis(if vaginal approach is used)
- 93. EUA GUIDELINES 2016 • Surgeons involved in VVF repair should have enough training, skills and experience to select an appropriate procedure for each patient. • Attention should be given to skin care, nutrition, rehabilitation counselling and support prior to and following fistula repair. • If a VVF is diagnosed within six weeks of surgery, consider catheterisation for 12 weeks after the causative agent.
- 94. • Tailor the timing of fistula repair to the individual patient and surgeon requirements once any oedema, inflammation and tissue necrosis or infection, are resolved. • Where ureteric re – implantation or augmentation cystoplasty are required, the abdominal approach is necessary. EUA GUIDELINES 2016
- 95. 6.Ensure that the bladder is continuously drained following fistula repair until healing is confirmed • (10-14 days for simple and/or postsurgical fistulae; • 14-21 days for complex and/or post-radiation fistulae). 7.If urinary or faecal diversions are required, avoid using irradiated tissue for repair. 8.Use interposition grafts when repair of radiation associated fistulae is undertaken. EUA GUIDELINES 2016
