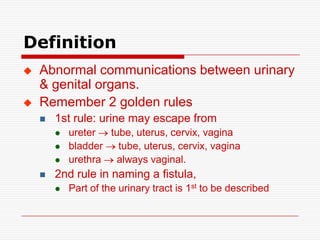
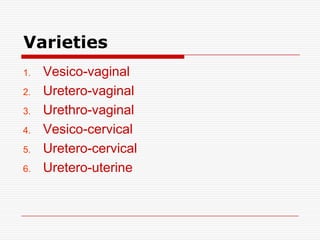
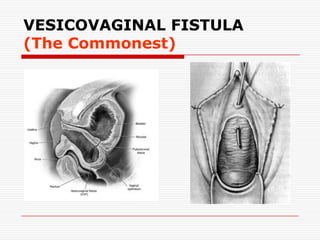
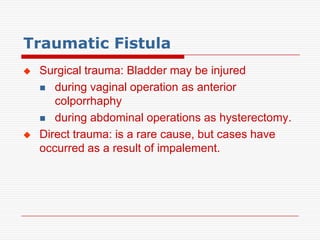
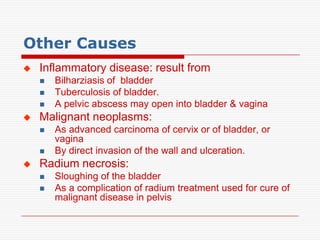
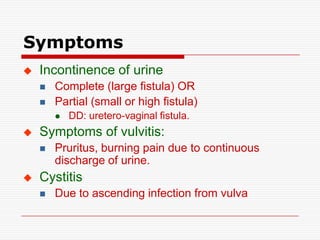
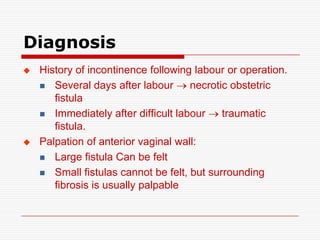
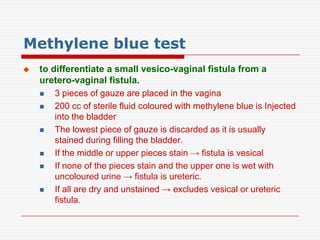
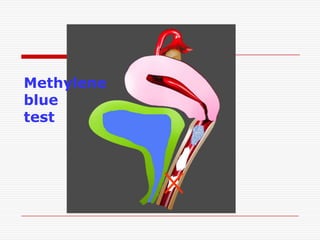
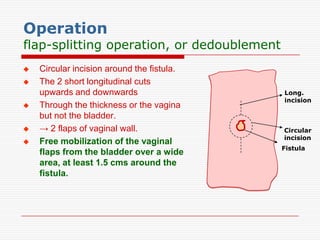
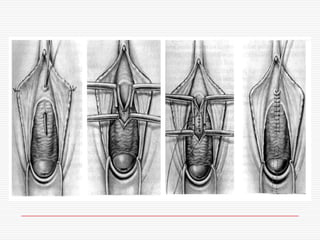
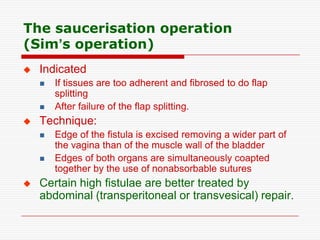
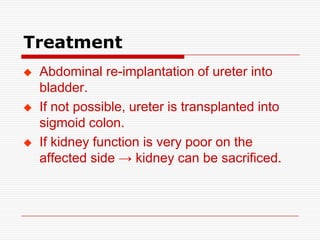
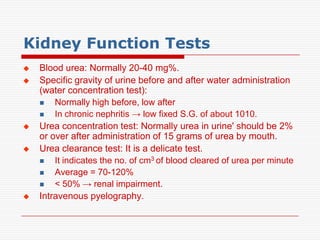
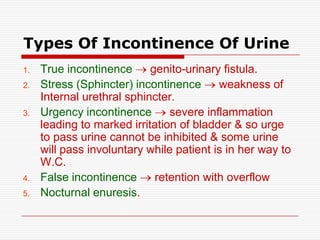
The document discusses genitourinary fistulas, which are abnormal connections between urinary and genital organs. It defines different types of fistulas including vesicovaginal, ureterovaginal, and urethrovaginal. The most common type is the vesicovaginal fistula, which is often caused by prolonged obstructed labor leading to tissue necrosis. Symptoms include urinary incontinence. Diagnosis involves history, examination for openings, and dye tests to locate the fistula. Management includes prevention of obstetric injuries, surgery to close openings, and postoperative catheterization.