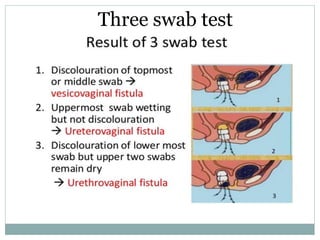
This document discusses genitourinary fistulas, including their classification, causes, symptoms, investigations, management, and prevention. The main types of fistulas are vesicovaginal, urethrovaginal, and ureterovaginal. Obstetric causes like obstructed labor are common in developing countries, while surgical trauma is more common in developed countries. Symptoms include continuous urine leakage. Investigations include dye tests and imaging. Management depends on the fistula type and complexity, and may involve surgical repair techniques like saucerization. Prevention focuses on adequate obstetric and surgical care to avoid injury.