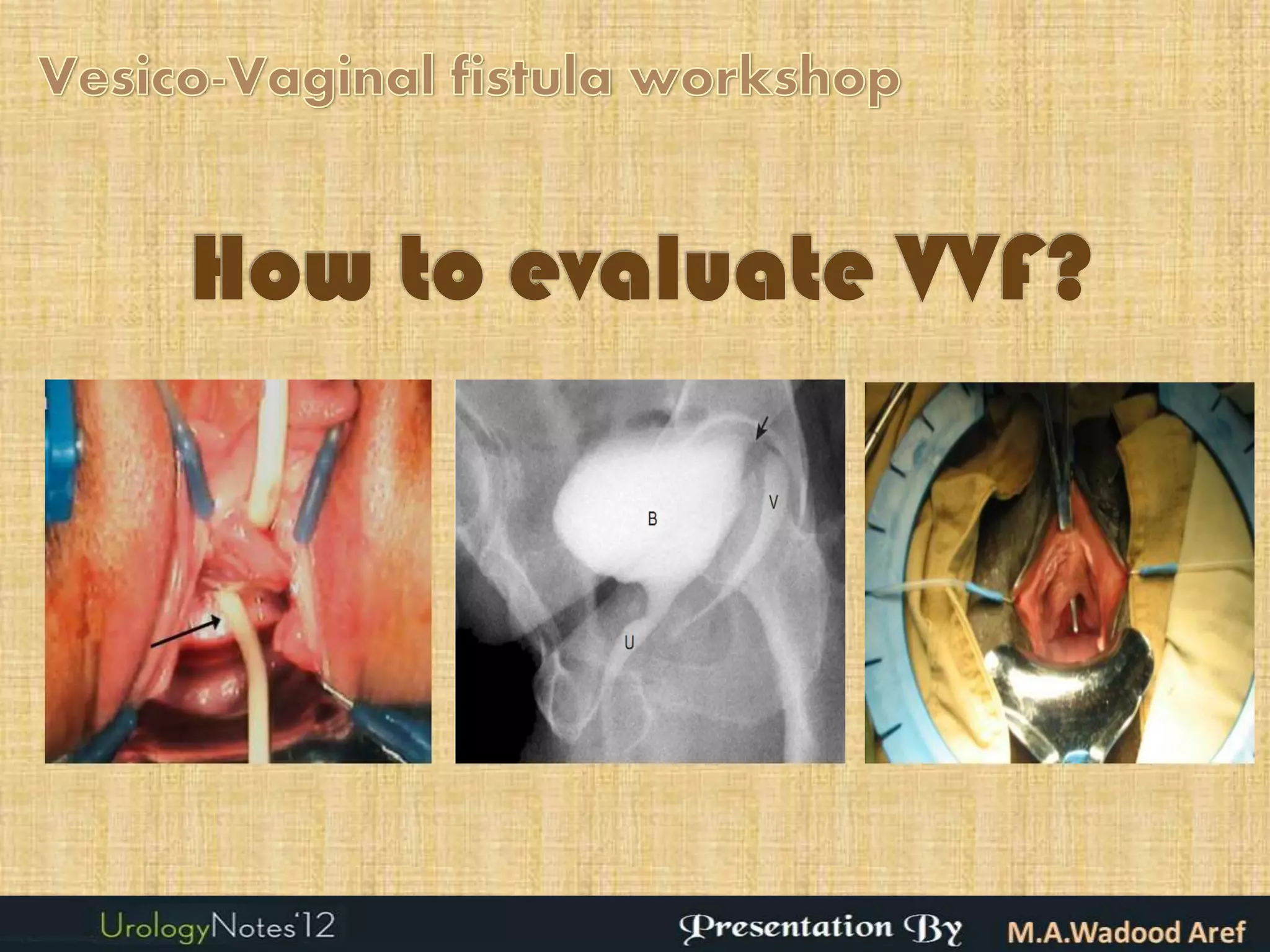
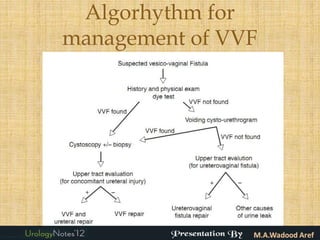
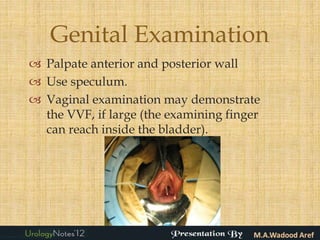
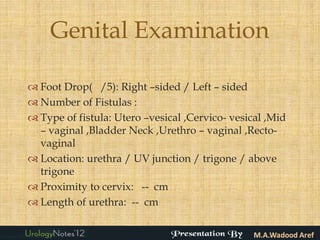
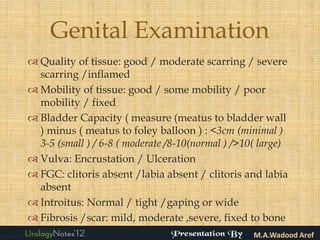
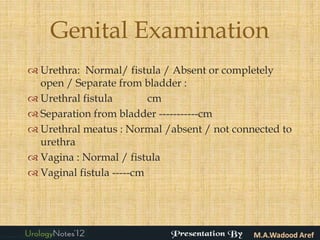
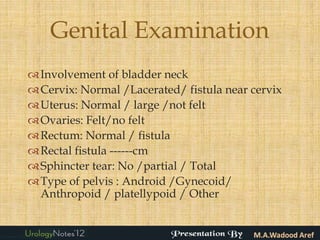
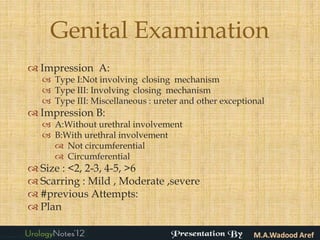
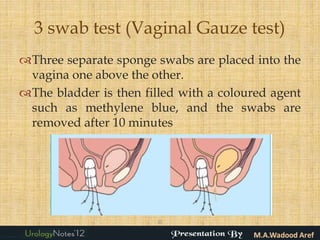
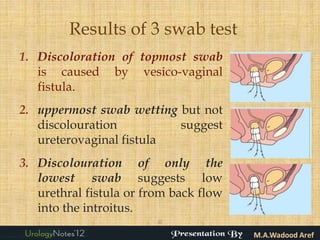
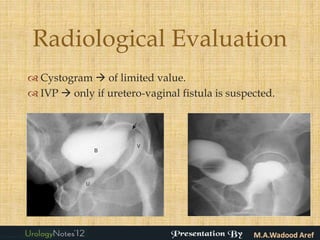
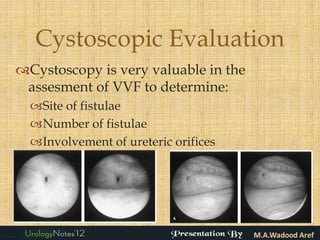
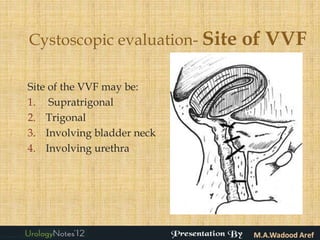
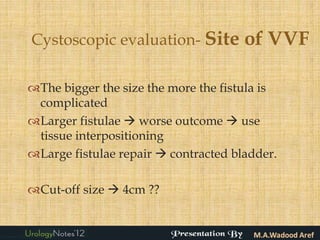
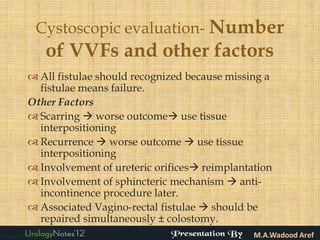
The document discusses the evaluation of vesicovaginal fistulas which includes obtaining a detailed medical history, performing a general and genital examination including a 3 swab test, and radiological evaluations like cystography and intravenous pyelography to determine the site, size, number and other characteristics of the fistula in order to inform the appropriate management approach. Cystoscopy is particularly useful for identifying the specific site of the fistula, whether additional fistulas are present, and if the ureteric openings are involved.