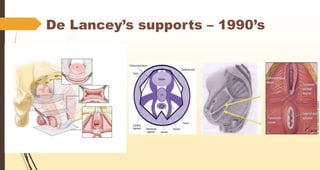
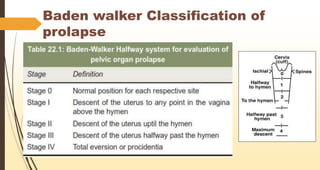
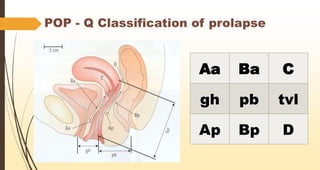
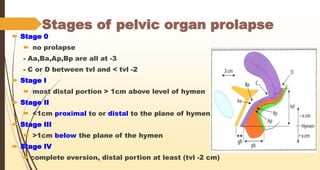
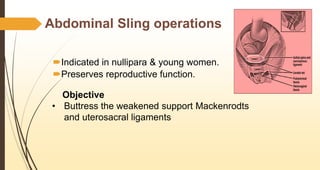
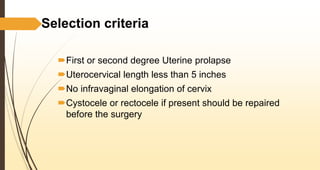
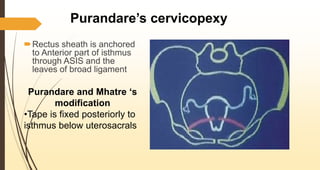
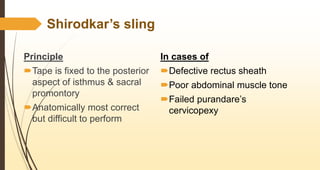
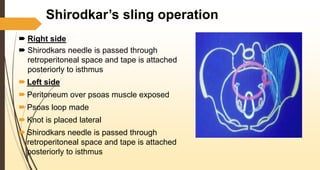
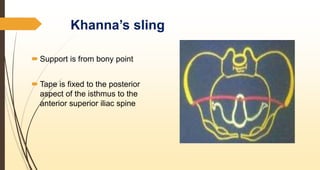
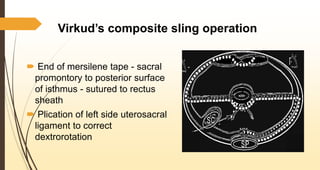
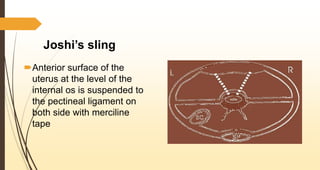
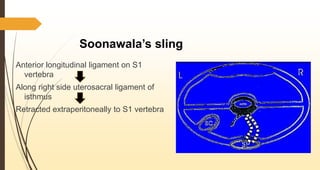
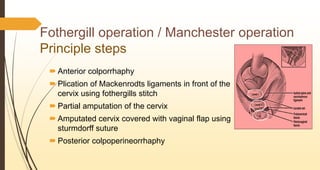
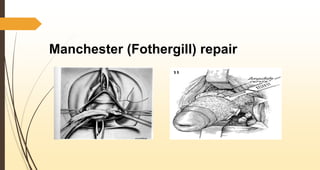
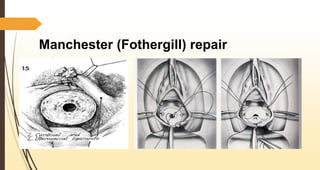
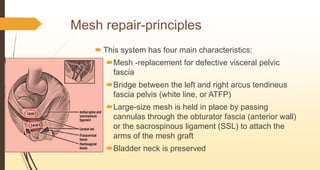
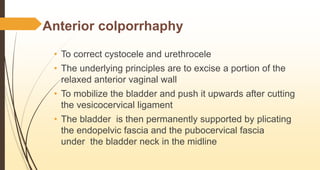
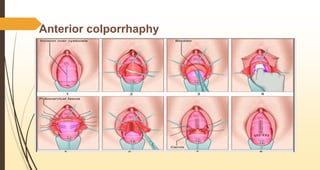
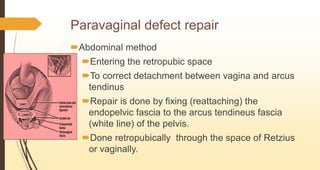
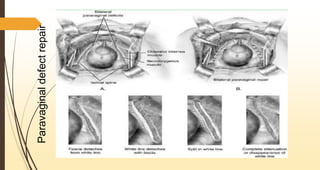
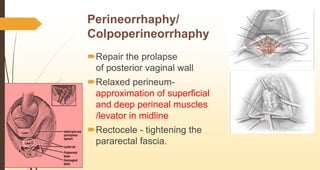
This document discusses various classifications and conservative surgical treatments for pelvic organ prolapse. It begins by describing the normal anatomical supports that prevent prolapse, including the bony scaffolding, endopelvic fascia, and pelvic musculature. It then covers several classification systems for prolapse, including the Baden-Walker and POP-Q systems. Conservative surgeries discussed include abdominal sling operations, various sling procedures, anterior and posterior colporrhaphies, paravaginal defect repairs, and perineorrhaphies. Newer procedures like vaginal sacrospinous cervico-colpopexy and posterior intravaginal slingplasty are also mentioned. The document emphasizes that hyster