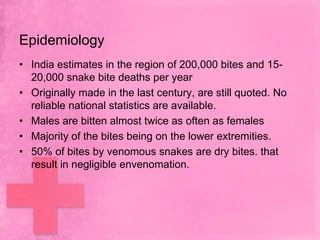
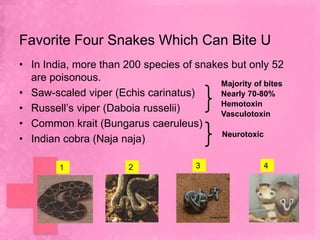
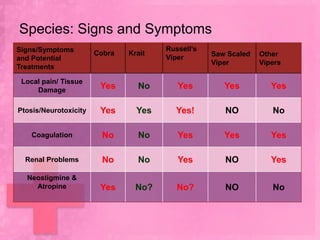
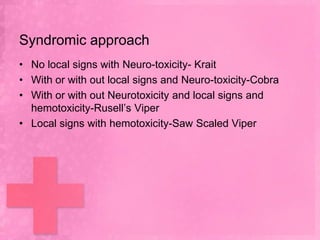
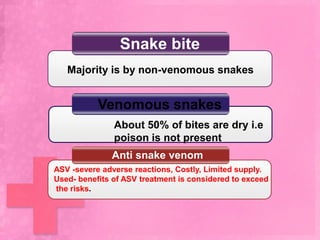
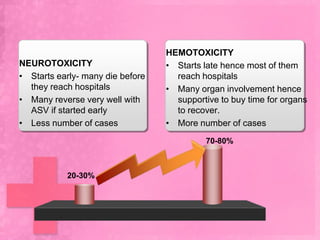
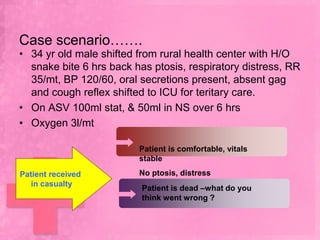
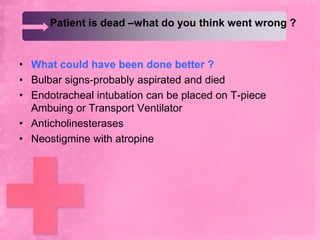
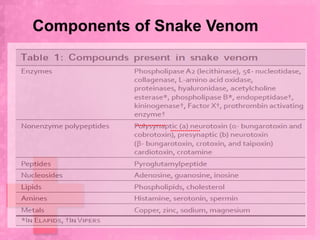
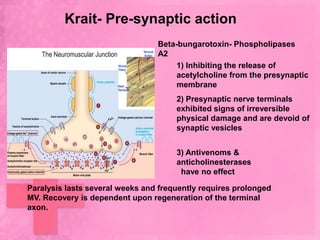
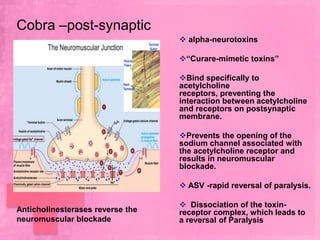
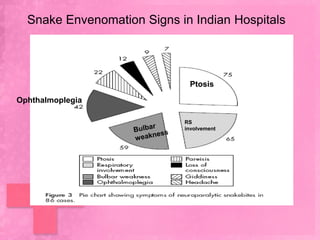
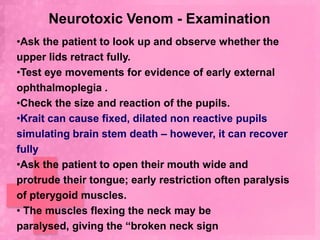
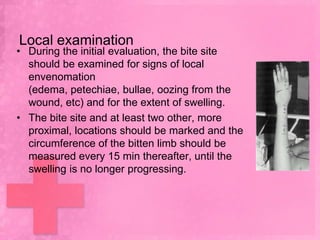
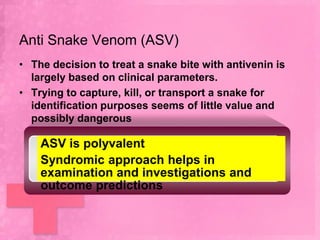
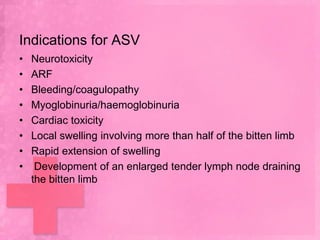
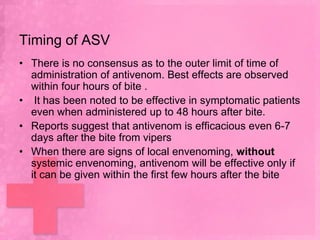
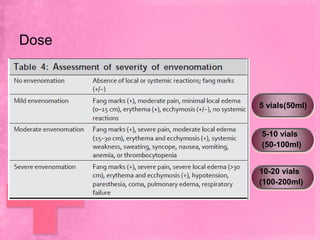
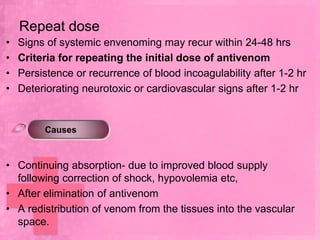
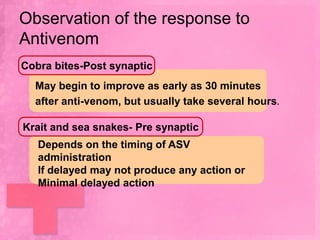
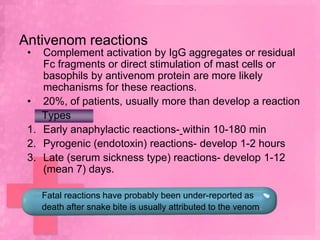
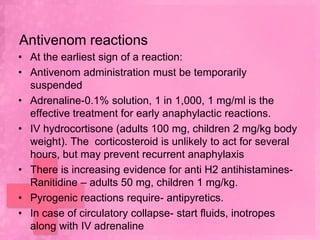
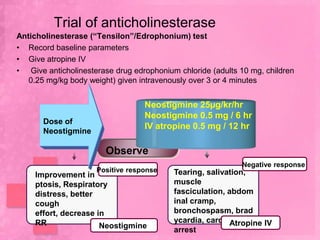
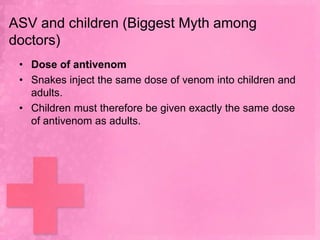
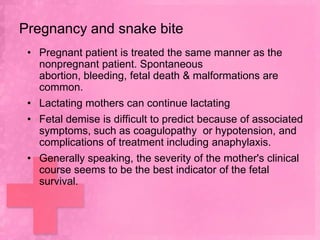
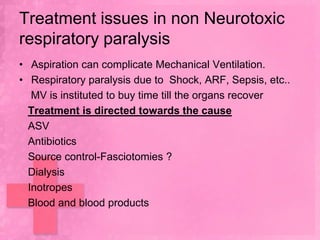
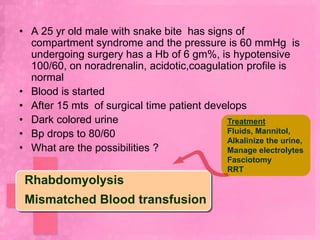
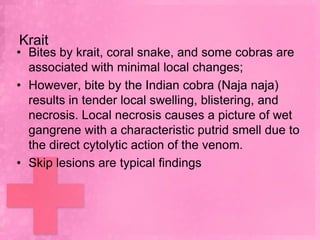
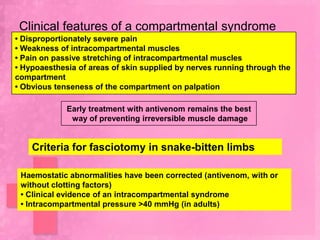
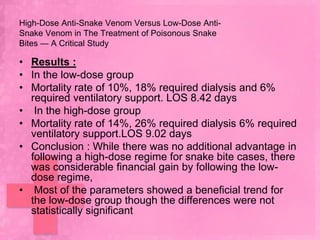
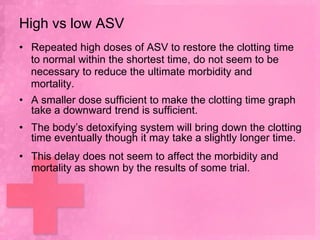
The document reviews the management of snake bite victims in India, highlighting the prevalence of snake bites and mortality rates, emphasizing that many bites are from non-venomous snakes or dry bites. It discusses the clinical features, treatment options such as anti-snake venom (ASV), indications for use, and the importance of timing in ASV administration. The document also covers complications associated with respiratory paralysis and the need for mechanical ventilation, as well as specific management protocols for different types of snake envenomation.