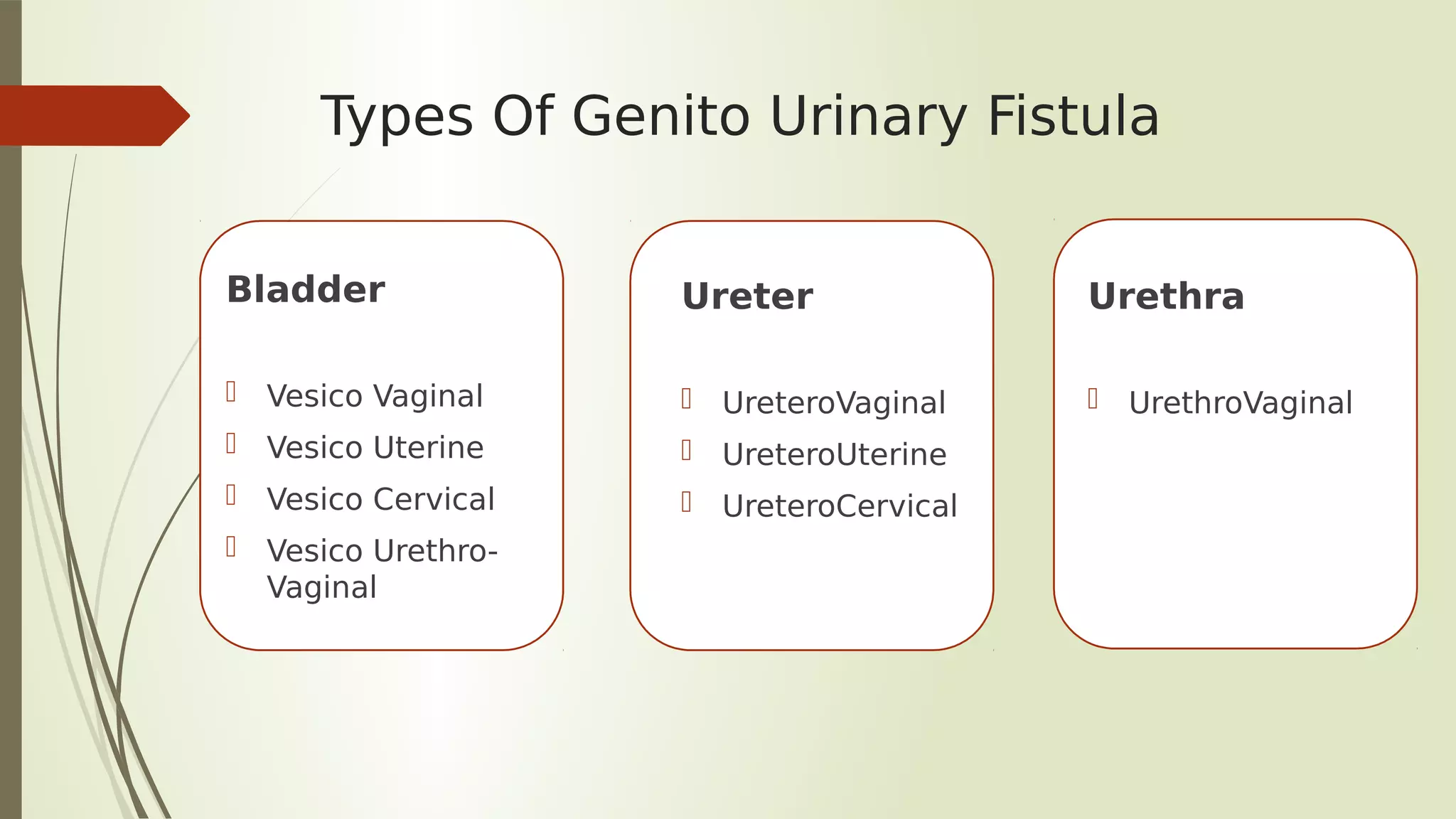
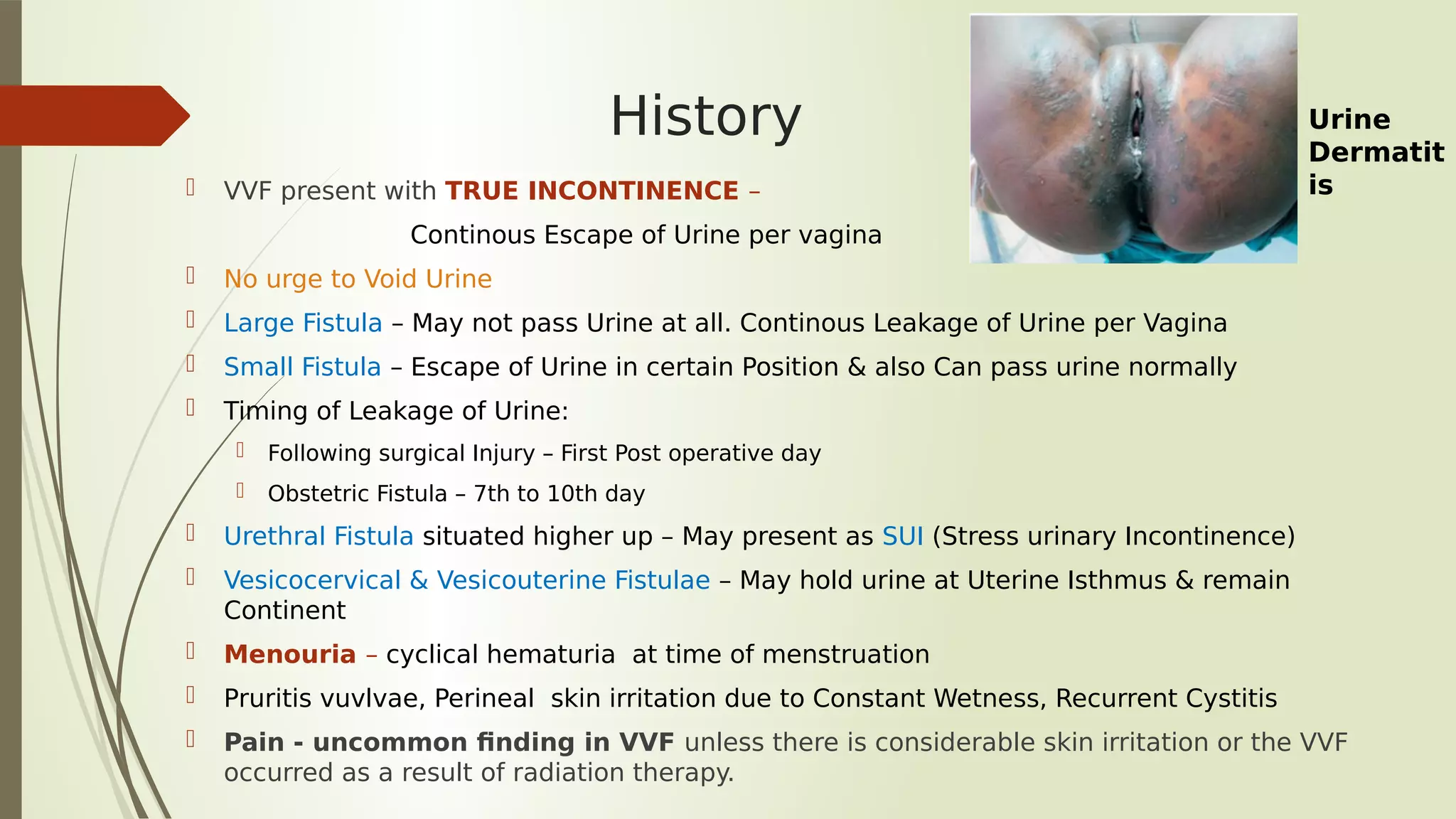
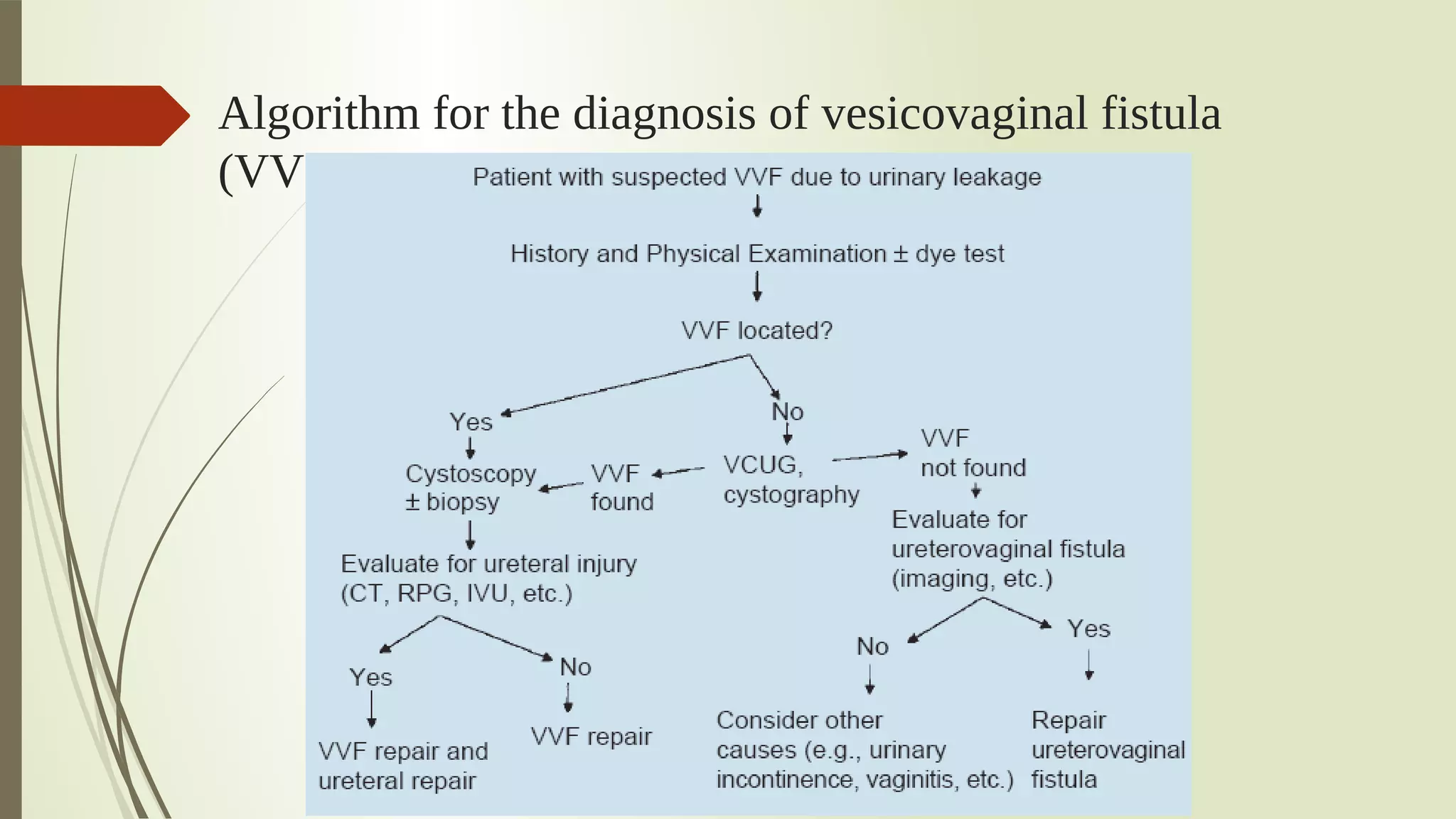
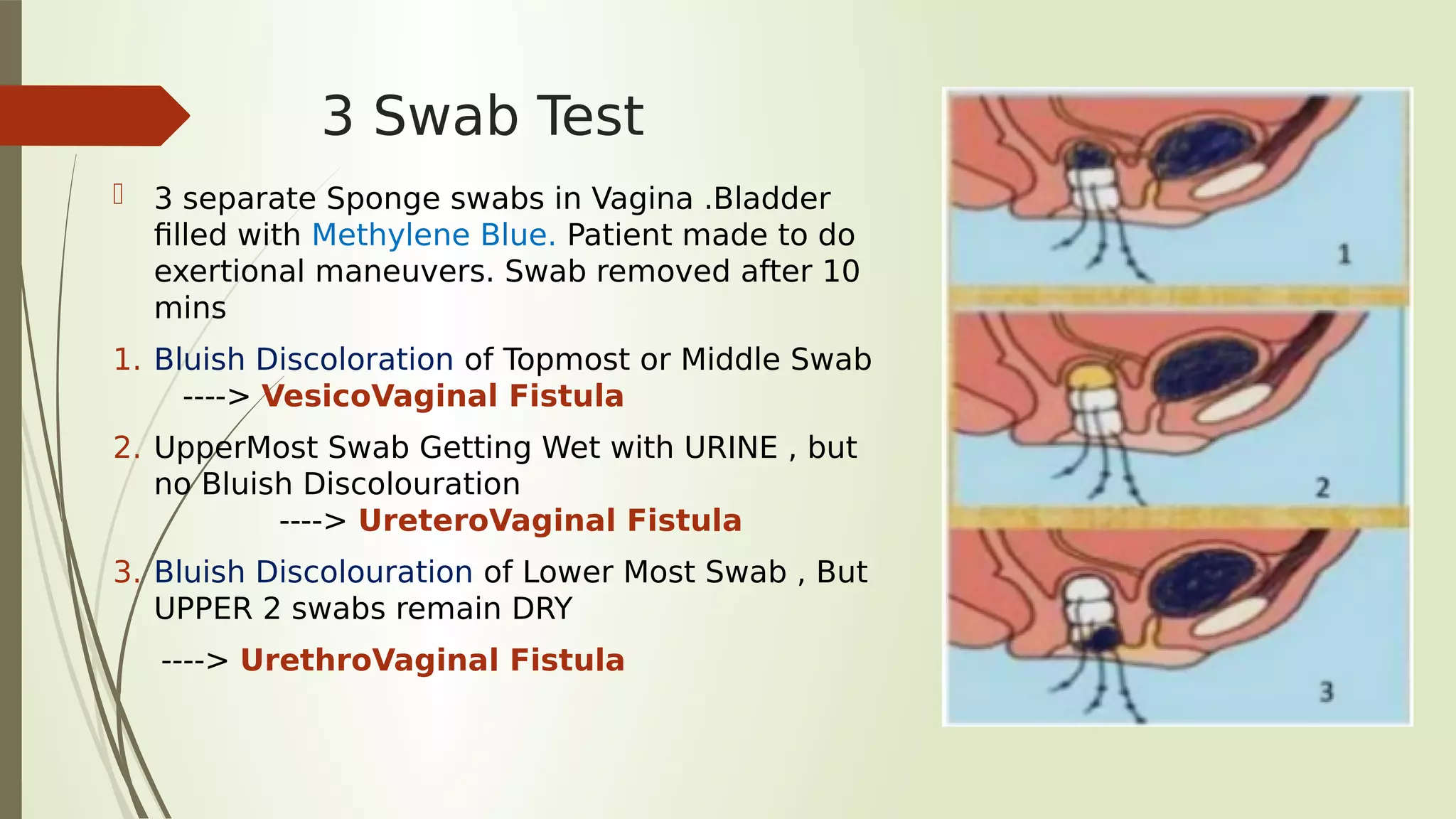
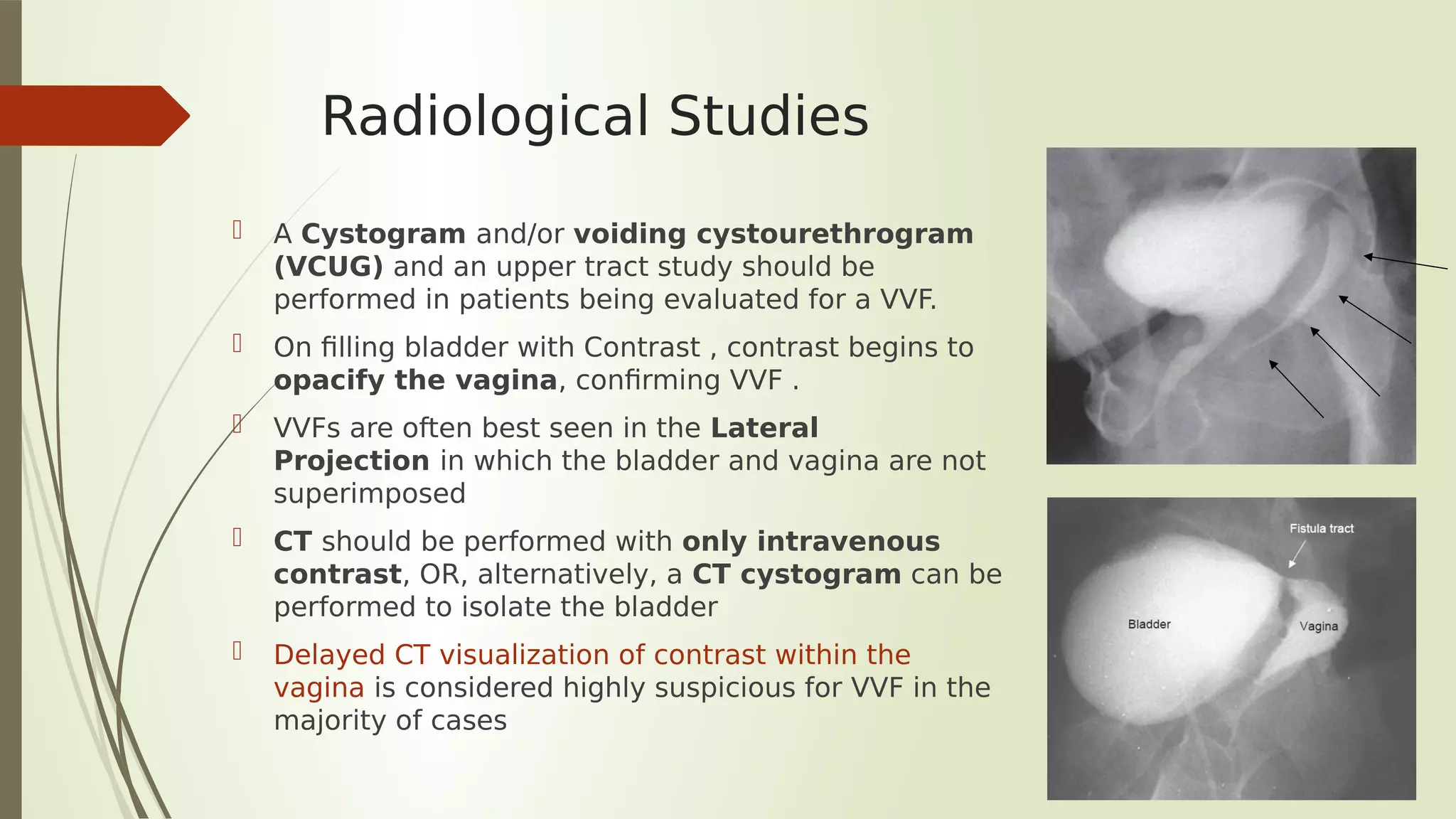
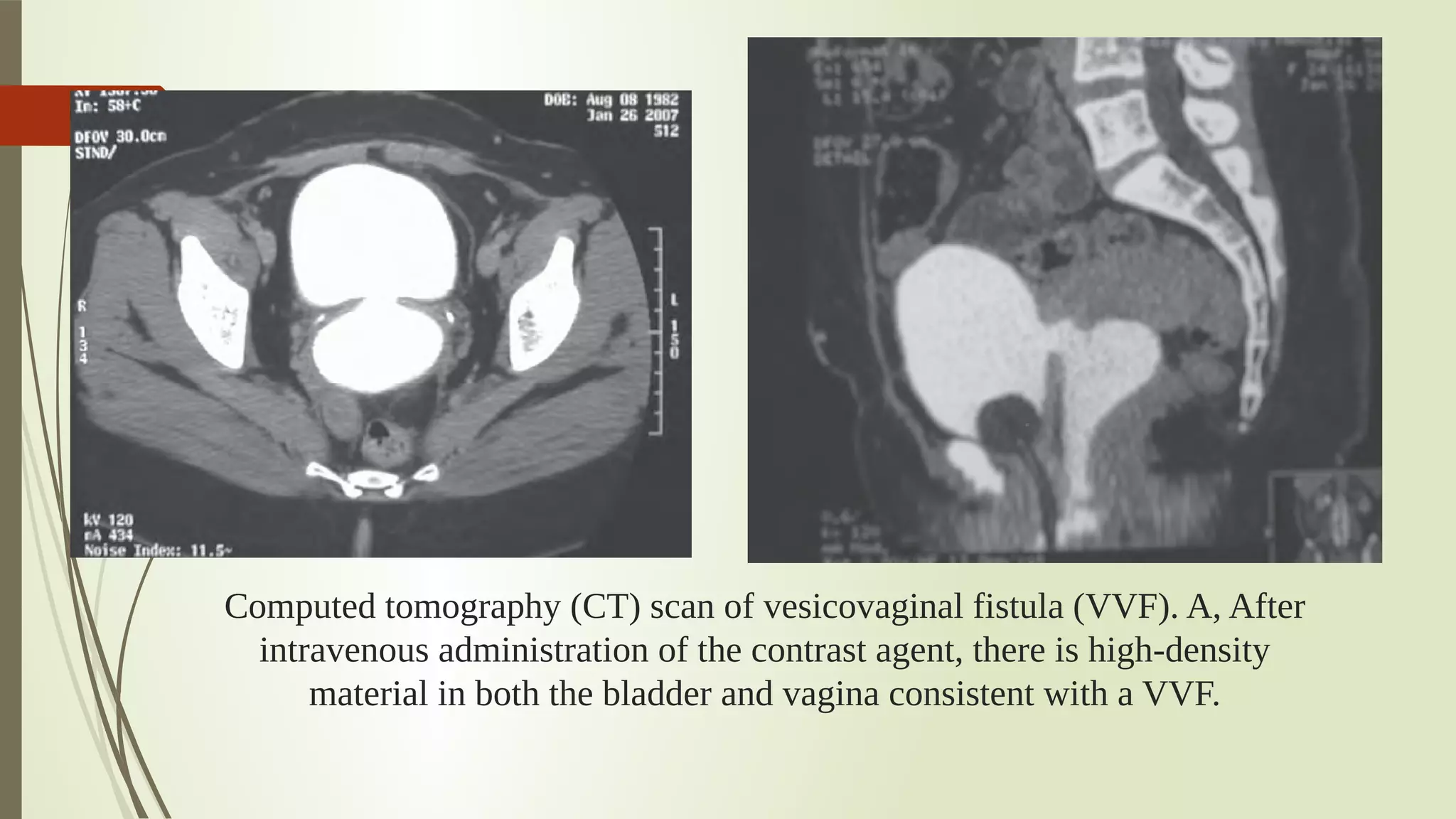
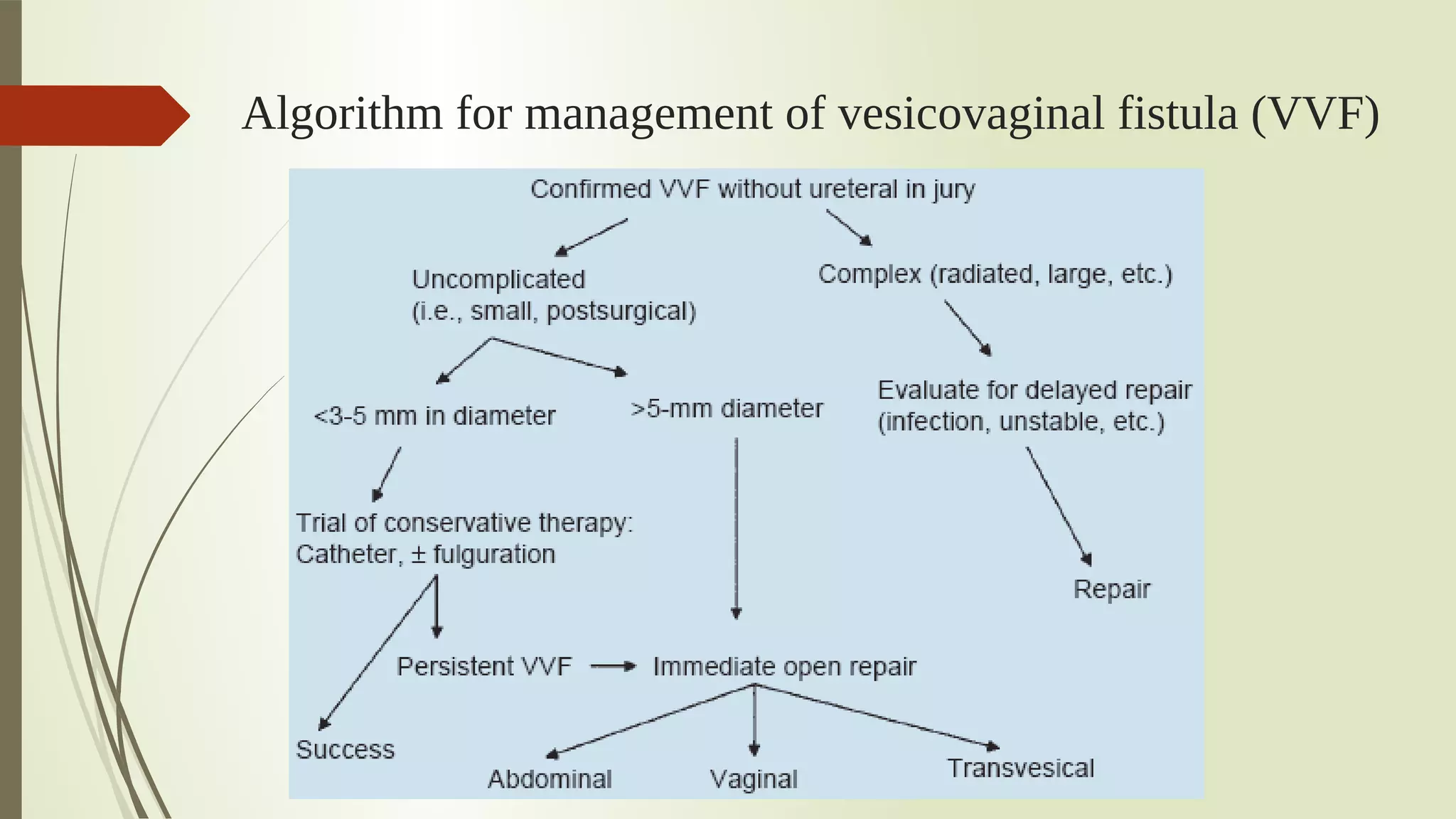
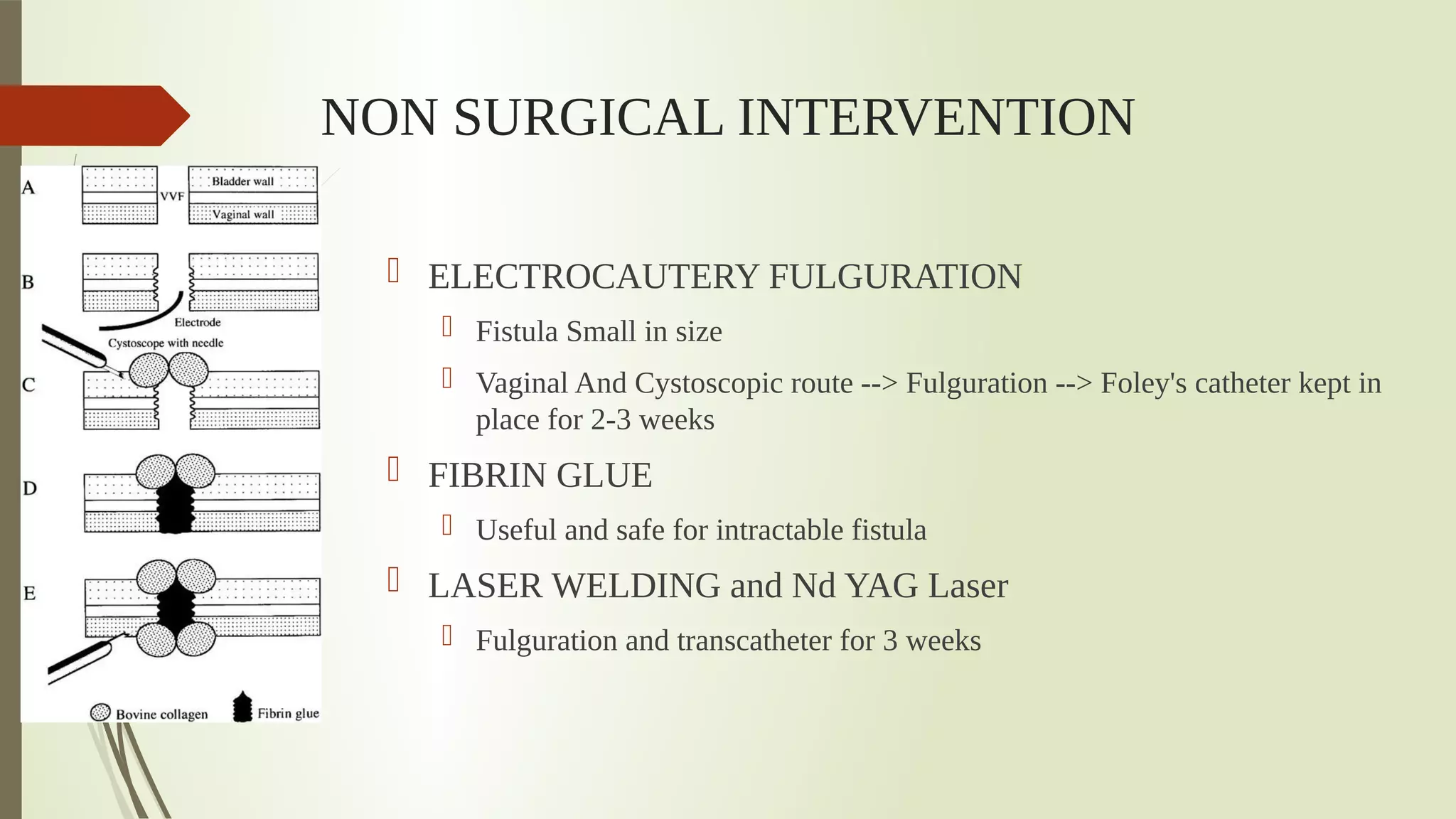
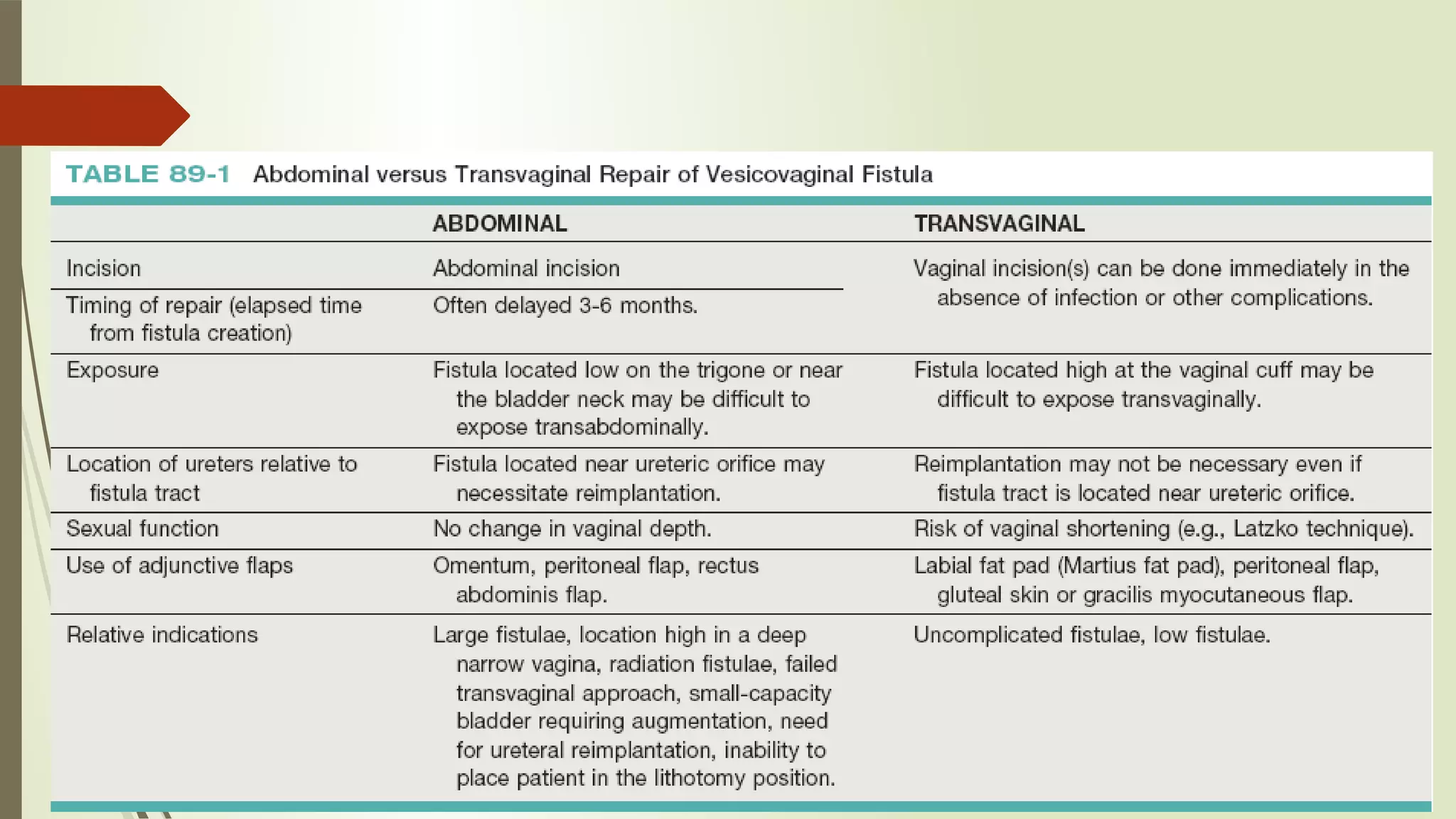
The document discusses urinary tract fistulas, focusing on urogenital fistula types, their etiology, especially obstetrical and surgical causes, and classifications related to location and size. Diagnosis and evaluation of vesicovaginal fistula (VVF) are outlined, including clinical history, examination methods, and radiological studies. Management options range from conservative and medical treatments to surgical interventions, emphasizing the importance of timely and appropriate repair approaches.