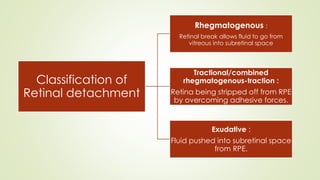
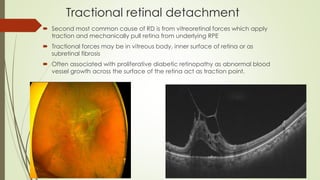
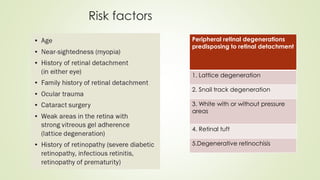
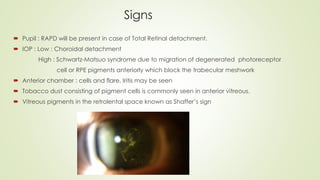
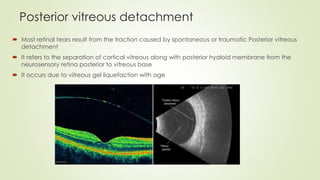
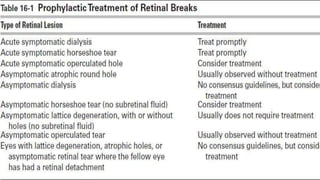
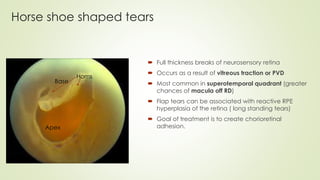
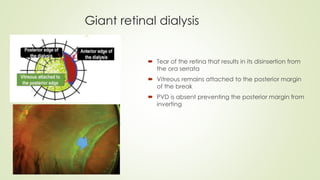
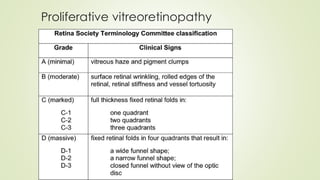
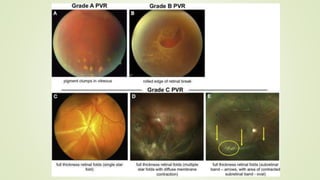
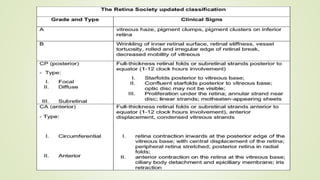
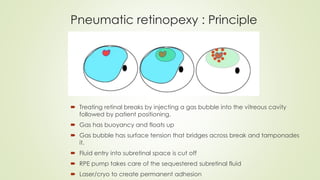
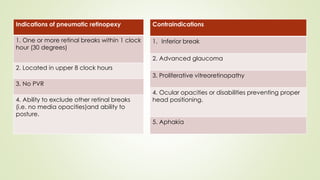
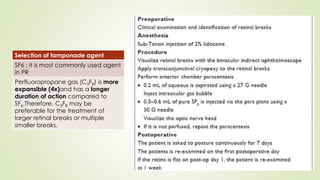
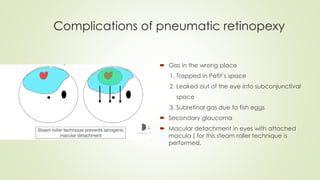
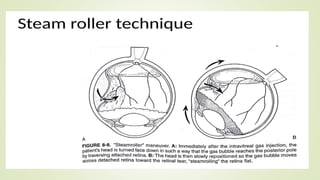
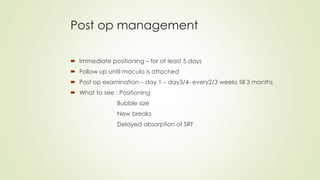
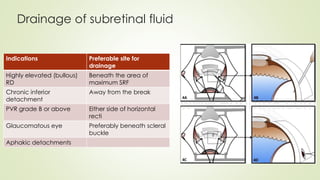
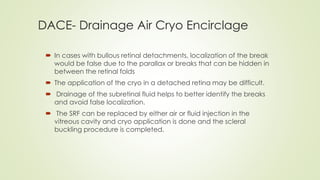
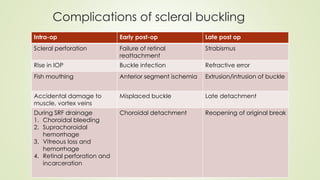
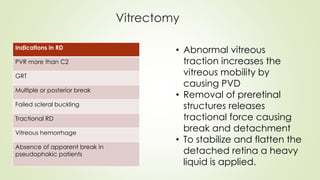
The document provides an in-depth overview of retinal detachment, including its classification into rhegmatogenous, tractional, and exudative types, along with associated risk factors and symptoms. It discusses various causes, management techniques such as pneumatic retinopexy and scleral buckling, and the surgical approaches to prevent or treat retinal detachment, emphasizing the importance of identifying retinal breaks. Additionally, it outlines postoperative management and potential complications arising from treatments, emphasizing the need for careful patient follow-up.