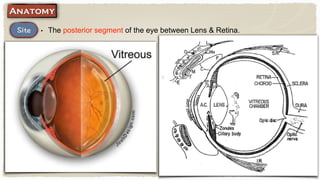
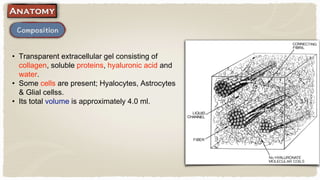
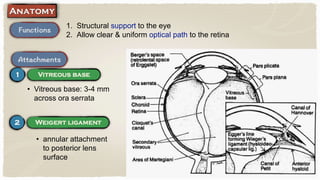
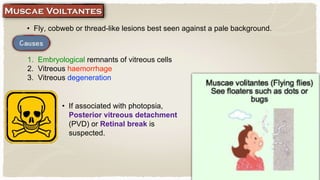
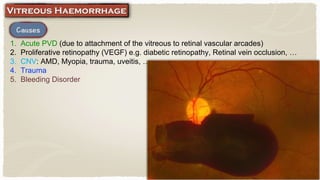
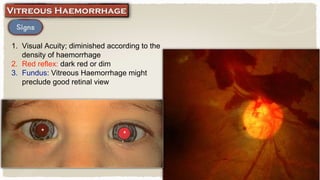
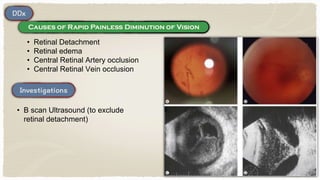
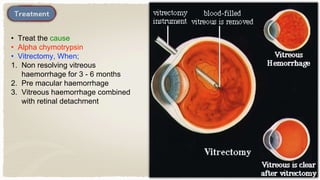
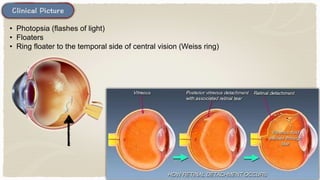
The vitreous is the transparent gel that fills the space between the lens and retina. It provides structural support to the eye and allows for a clear optical path. The vitreous can develop various lesions over time, which may be signs of vitreous degeneration or detachment from the retina. Vitreous hemorrhage occurs when blood leaks into the vitreous cavity, which can diminish vision depending on density and requires treatment if non-resolving.