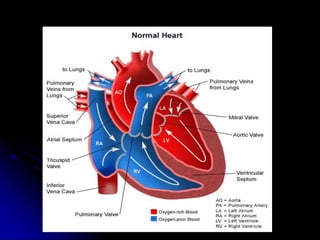
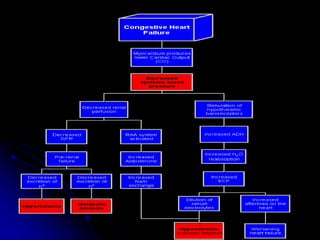
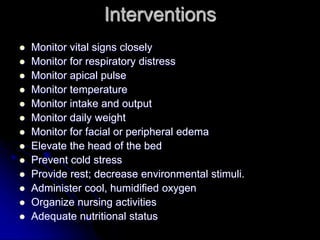
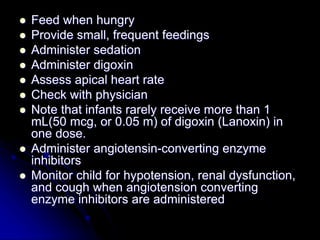
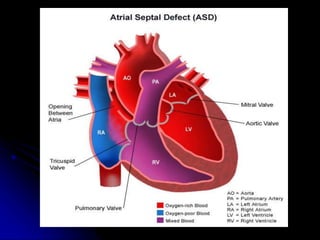
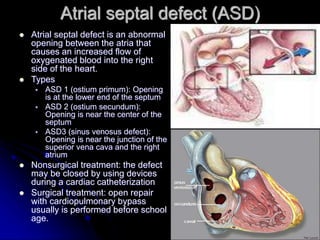
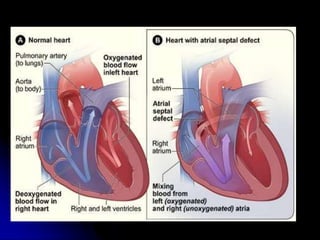
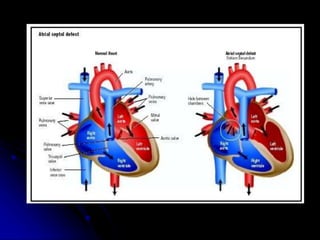
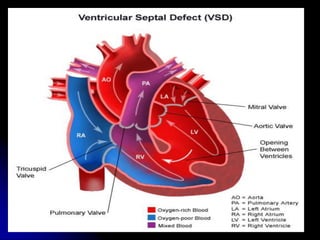
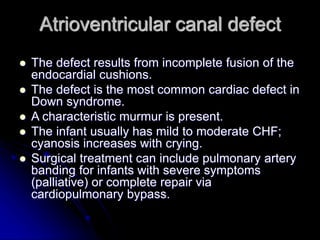
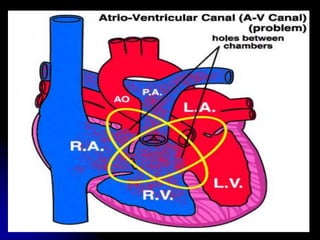
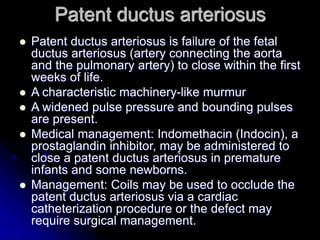
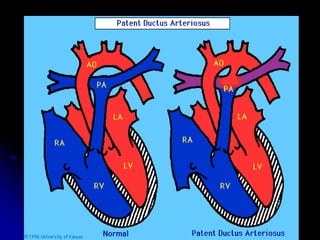
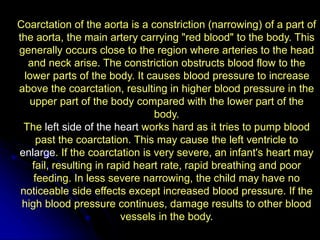
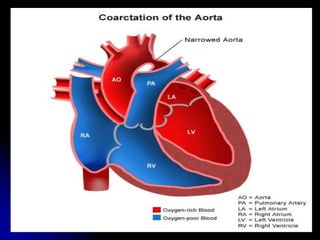
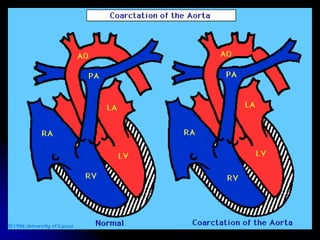
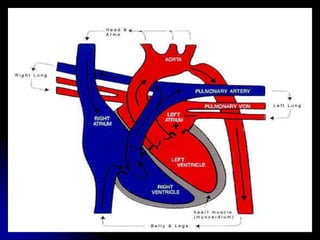
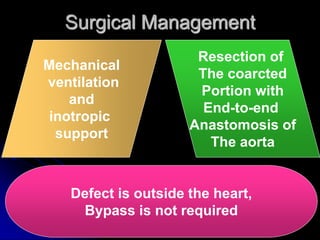
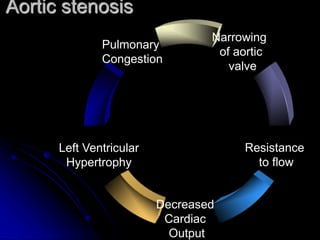
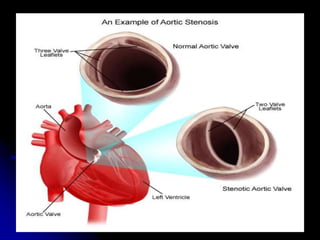
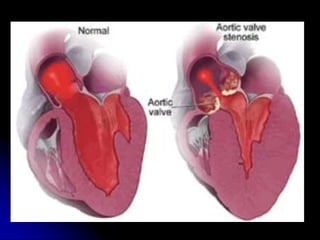
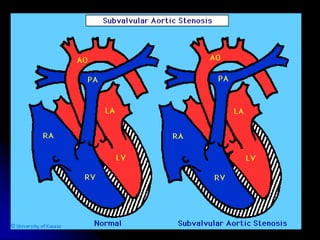
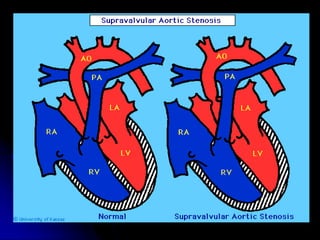
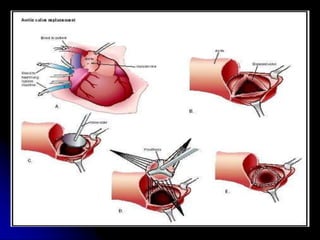
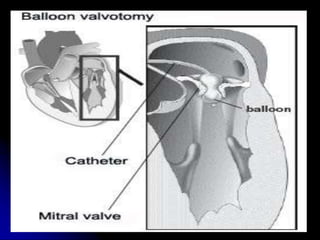
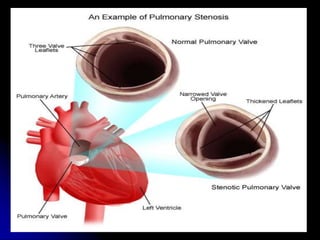
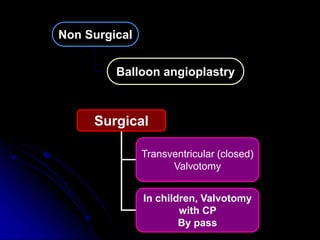
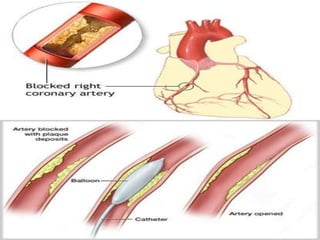
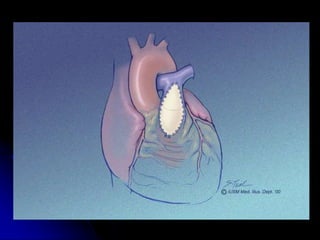
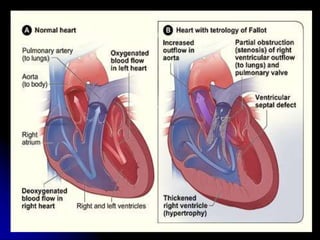
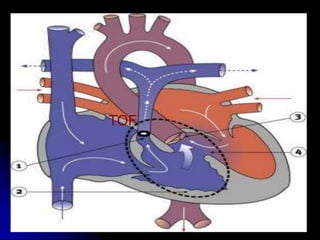
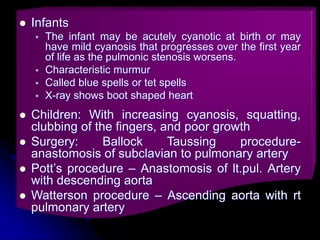
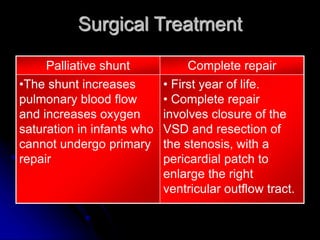
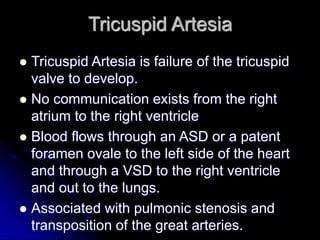
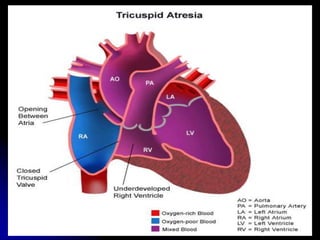
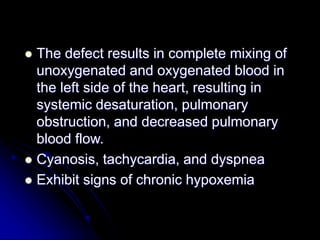
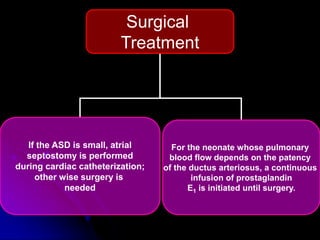
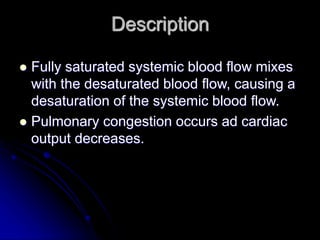
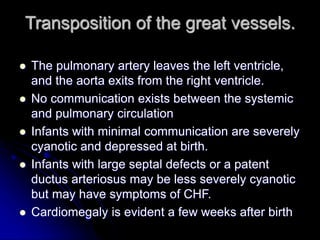
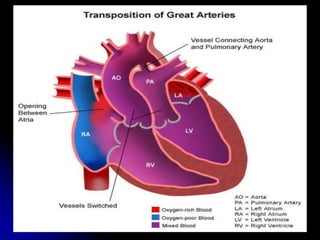
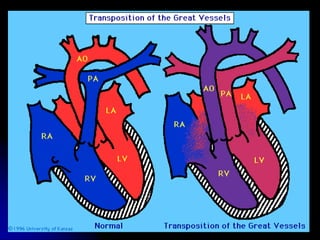
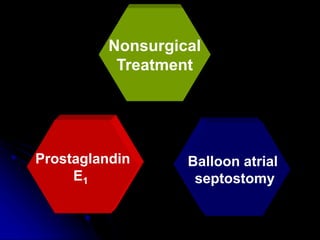
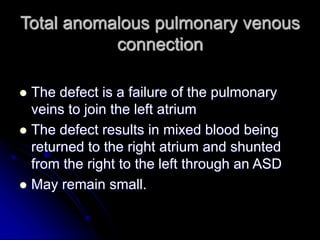
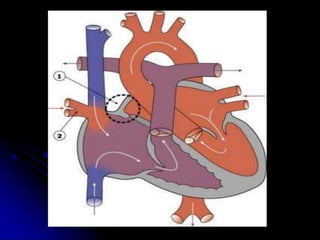
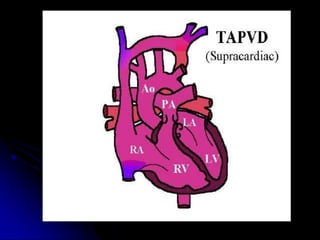
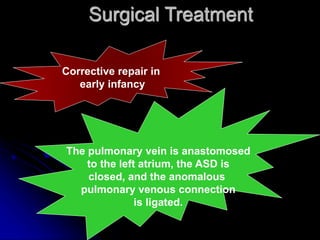
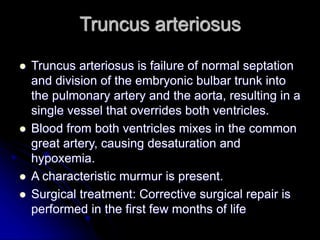
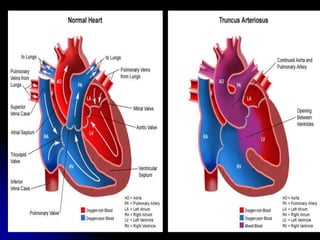
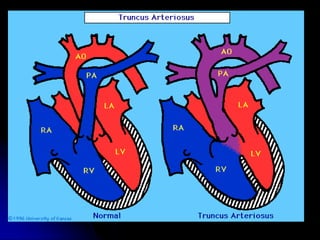
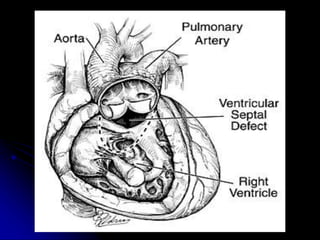
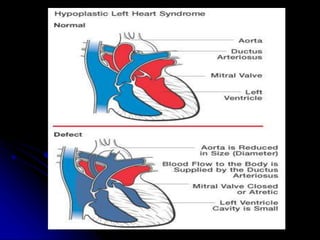
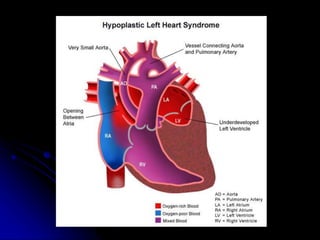
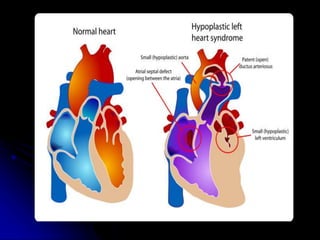
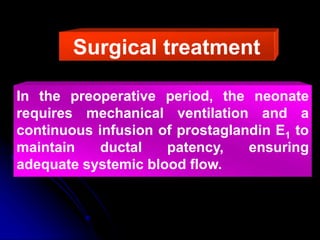
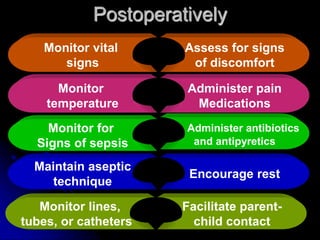
The document discusses various congenital heart defects that can cause congestive heart failure in infants and children. It describes defects that allow increased or decreased blood flow between the right and left sides of the heart, as well as obstructive defects. For each defect, it outlines characteristics, potential treatments such as surgery or catheterization, and nursing considerations. The overall goals of treatment are to improve cardiac function, remove fluid, decrease cardiac demands, improve oxygenation, and decrease oxygen consumption.