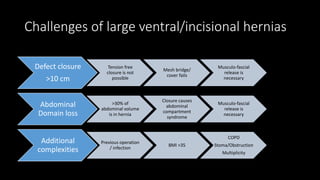
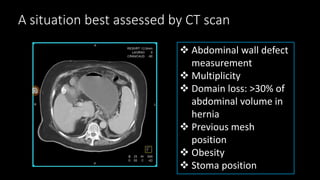
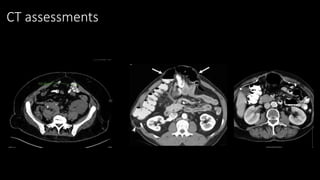
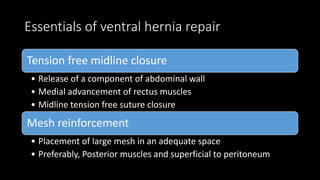
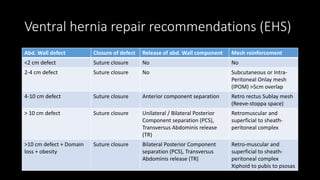
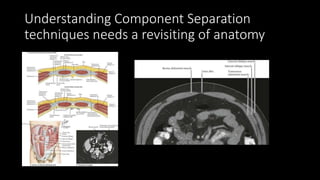
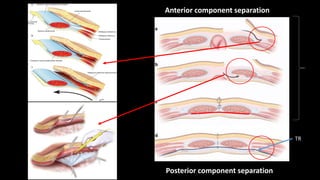
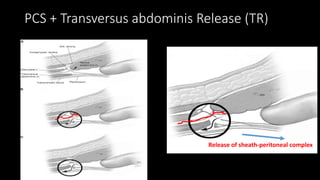
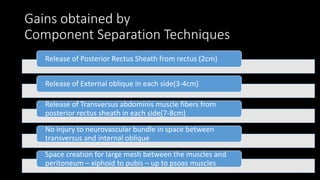
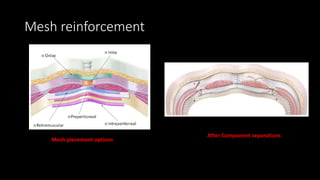
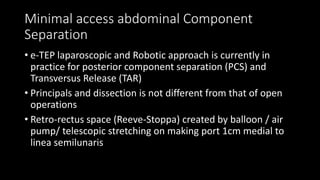
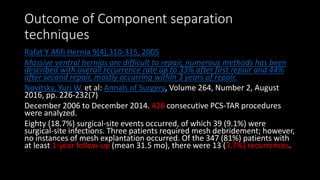
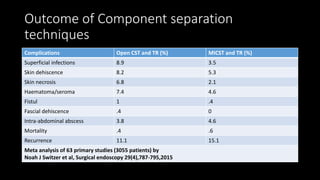
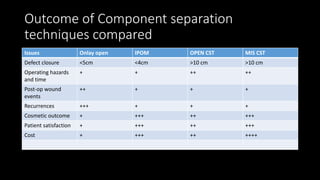
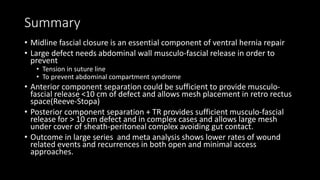
The document discusses the challenges and techniques of abdominal wall component separation for large ventral hernia repair, highlighting the necessity of musculo-fascial release and mesh reinforcement for successful outcomes. It reviews various repair techniques based on defect size and patient factors, with evidence suggesting improved post-operative outcomes with refined strategies. Additionally, it emphasizes the importance of understanding anatomical orientations and the potential benefits of minimally invasive surgery in hernia management.