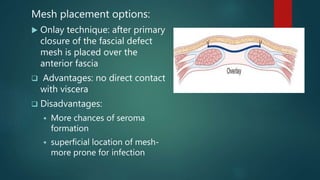
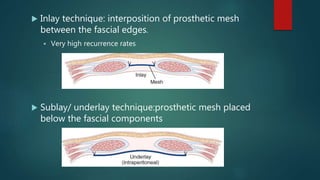
Ventral hernias occur when abdominal contents protrude through weaknesses in the abdominal wall. There are several types of ventral hernias including umbilical, epigastric, incisional, and parastomal hernias. Umbilical hernias are common in infants and adults, especially pregnant women or obese individuals. Epigastric hernias occur through the linea alba. Incisional hernias develop through surgical scars. Treatment depends on hernia size but may involve weight loss, mesh repair, or laparoscopic surgery. Proper surgical technique and prevention of postoperative infections can help reduce incisional hernia risk.