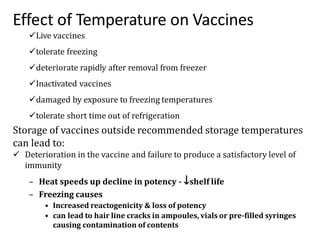
The cold chain refers to maintaining vaccines within the recommended storage temperature range of 2°C to 8°C during transport and storage until administration. This is important to ensure vaccine efficacy and potency. Live vaccines can tolerate freezing but are damaged by heat, while inactivated vaccines cannot tolerate freezing but can withstand short periods out of refrigeration. Strict temperature control is required during receipt, transport, storage at vaccination sessions, and disposal of vaccines to maintain their effectiveness.