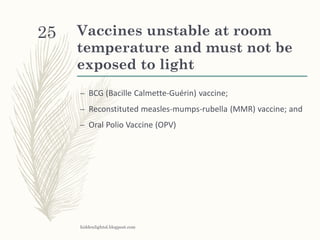
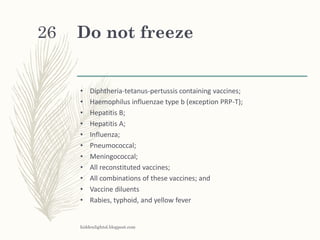
Vaccines must be kept within a narrow temperature range to remain effective. This document discusses the "cold chain" system used to transport and store vaccines between 2-8°C from manufacture to administration. It describes different vaccine types and the importance of proper storage in refrigerators, cold boxes, or freezers. Temperature monitoring using devices like data loggers is crucial to ensure potency. Exposure to heat, light, or freezing can damage vaccines, so procedures must be followed carefully when handling or transporting them.