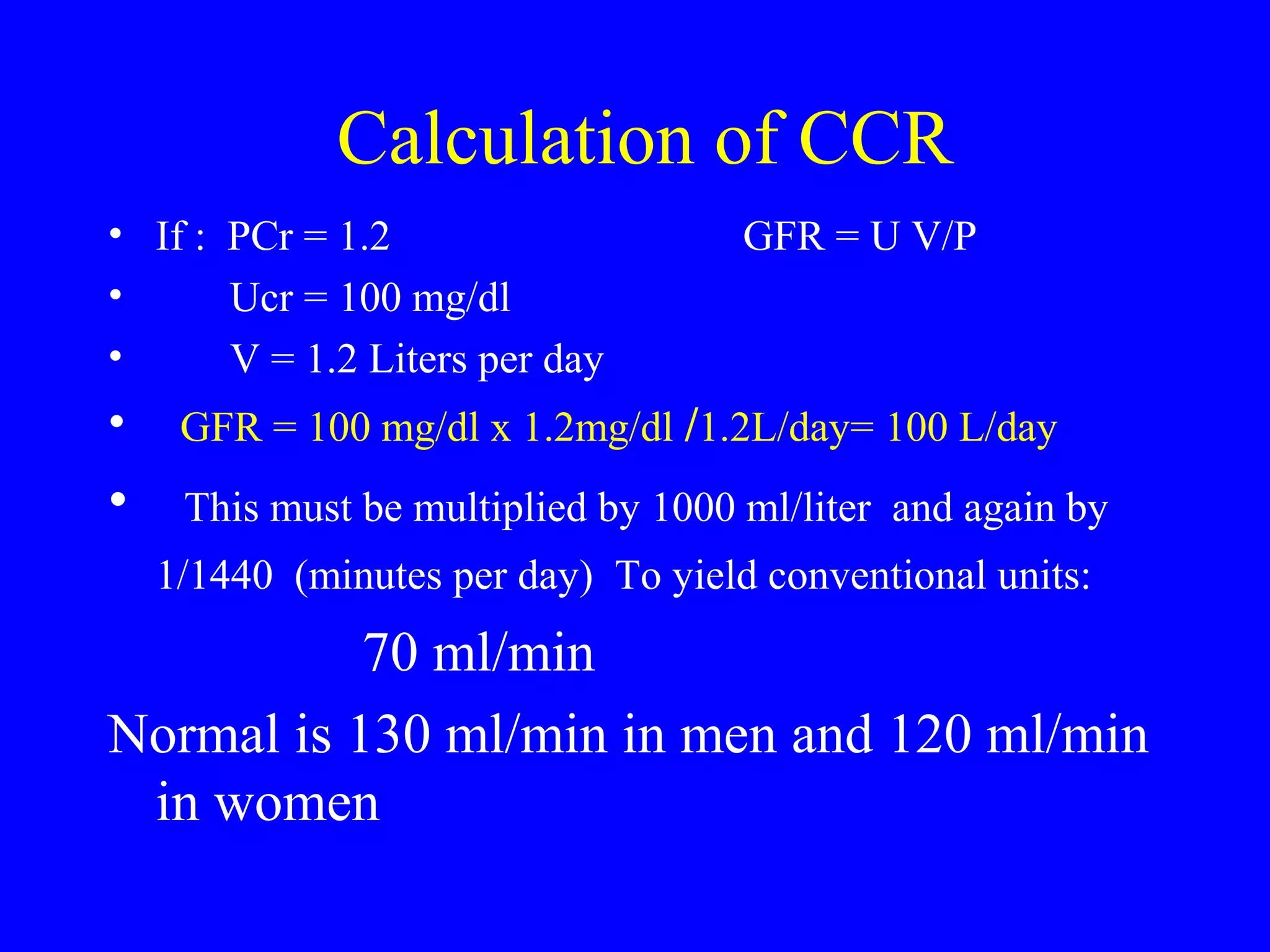
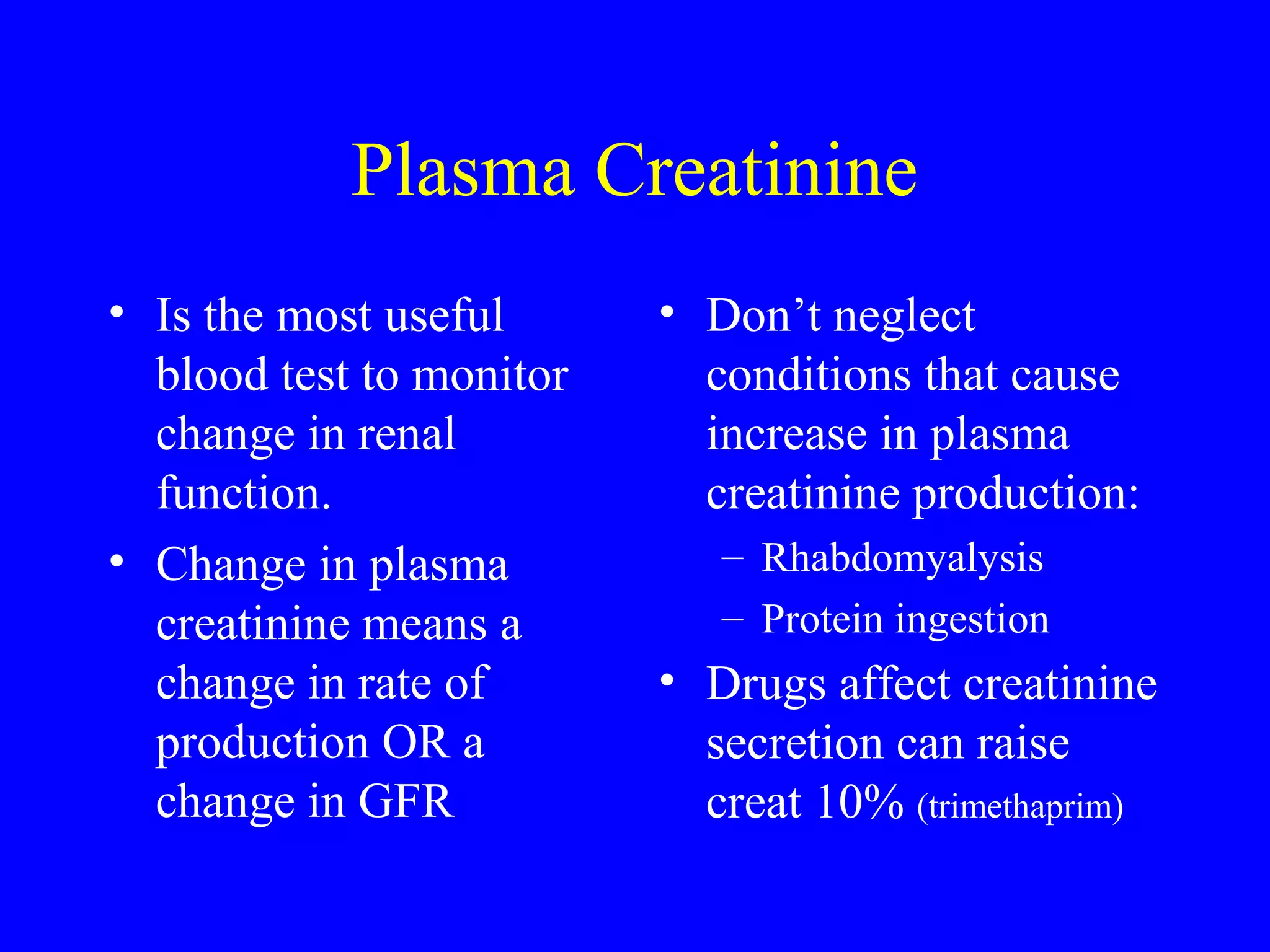
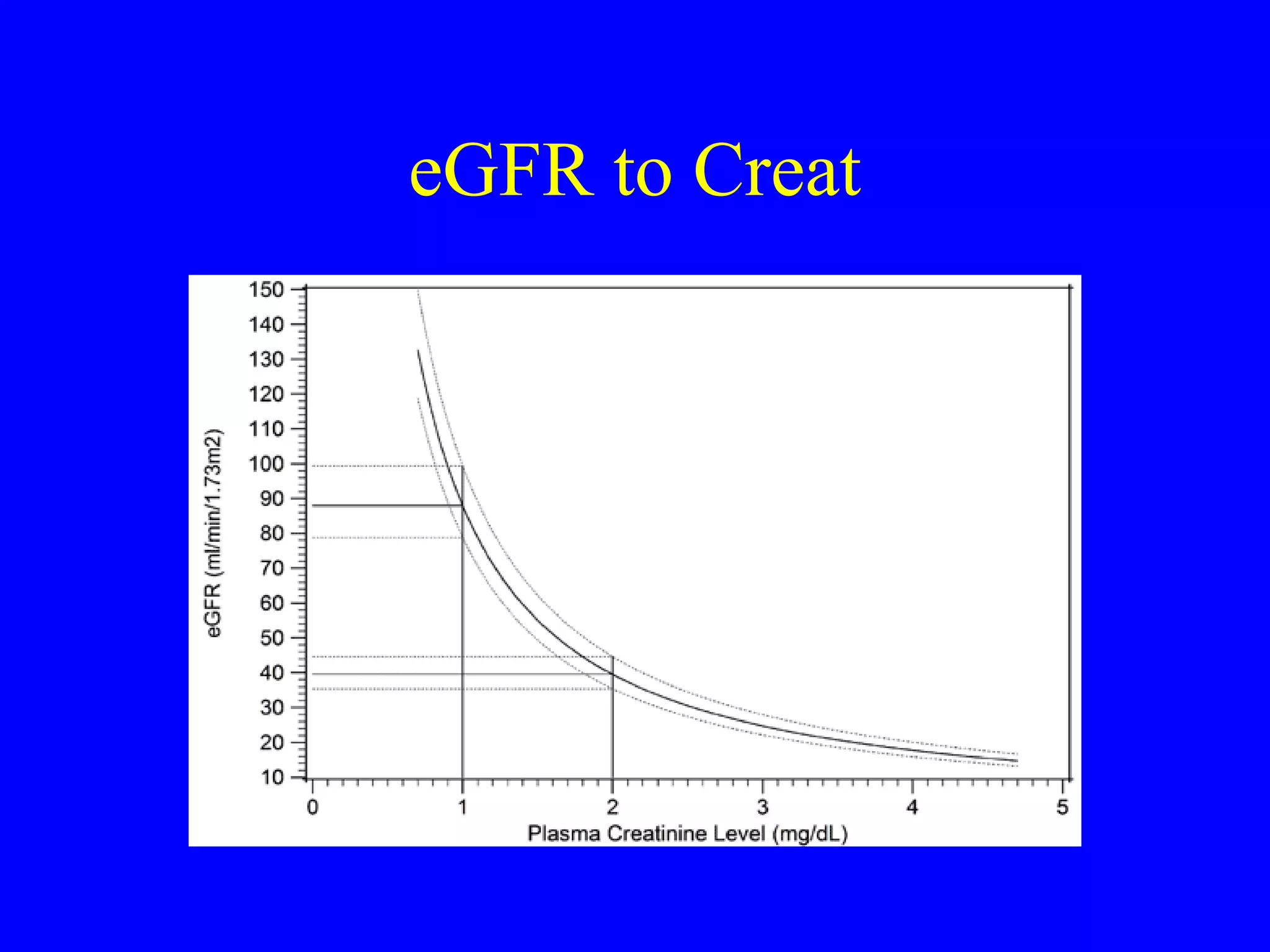
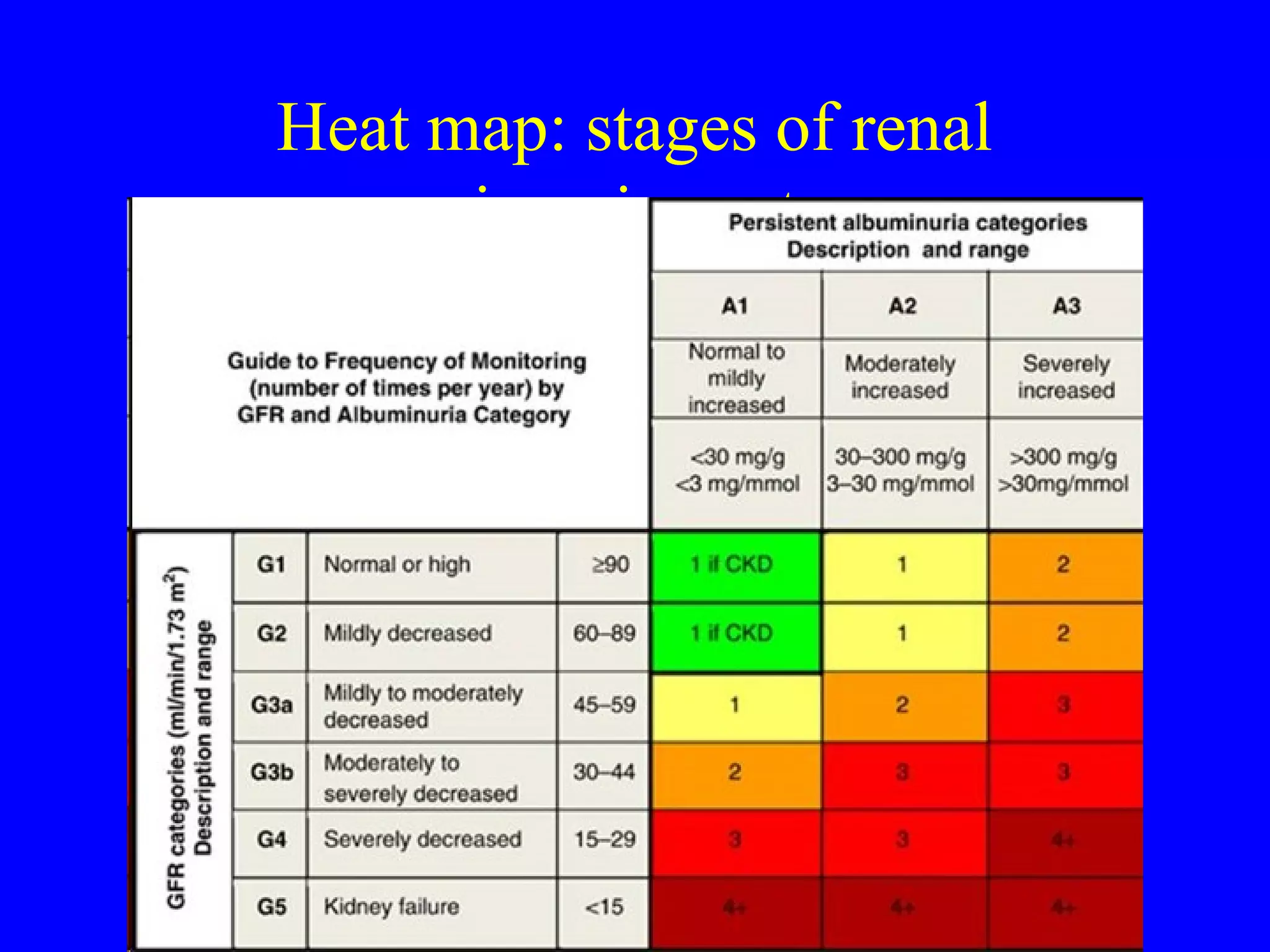
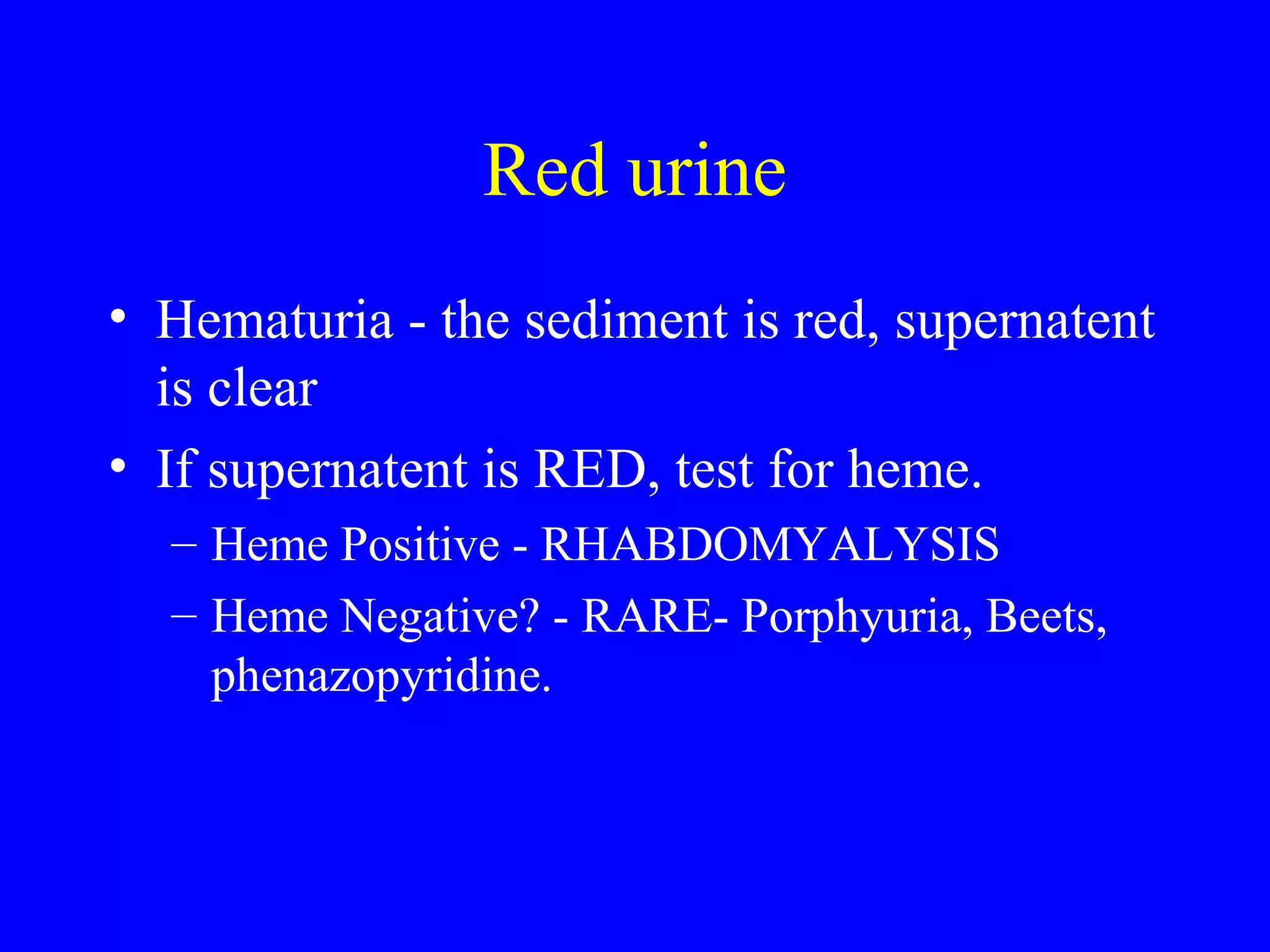
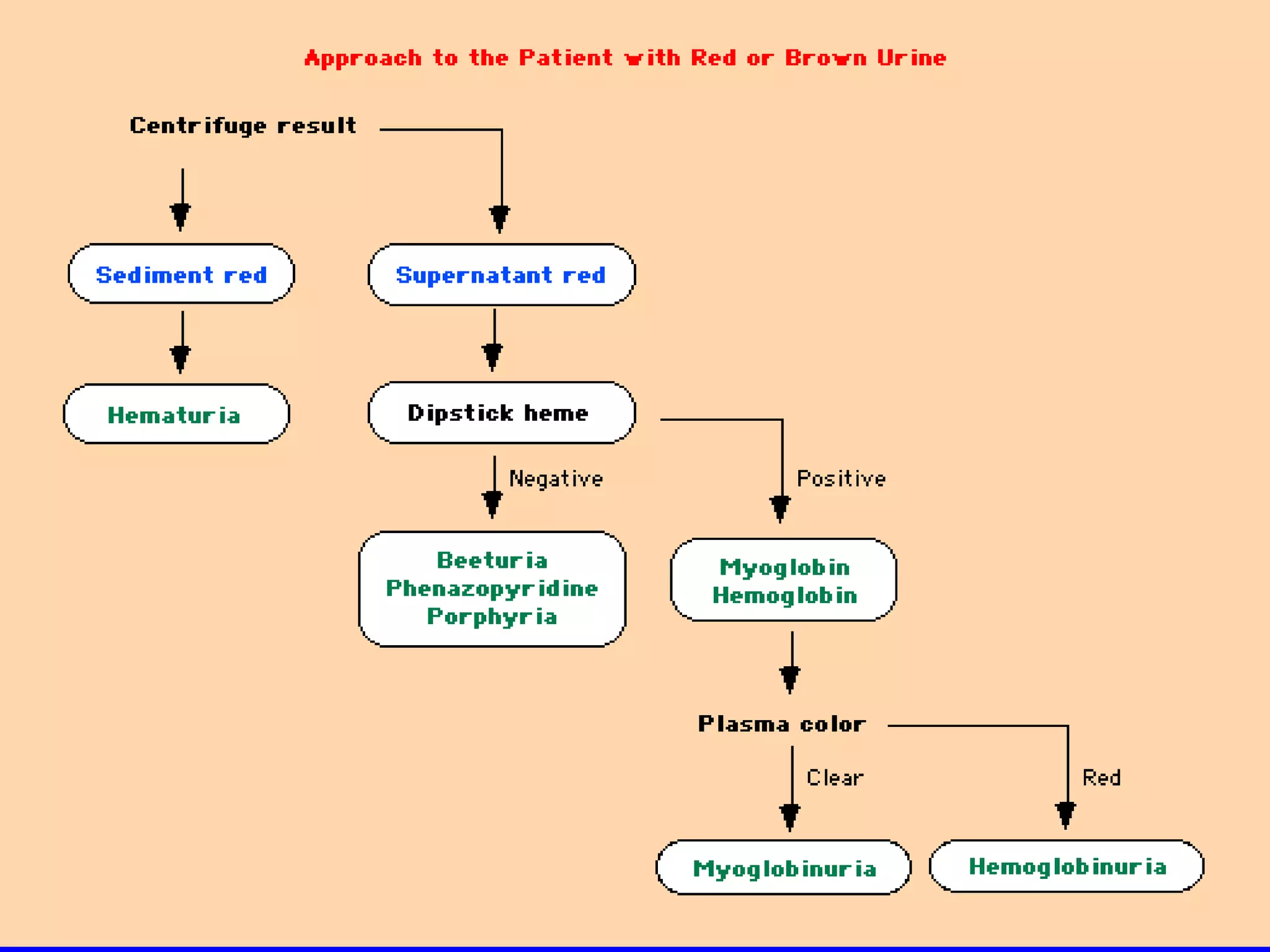
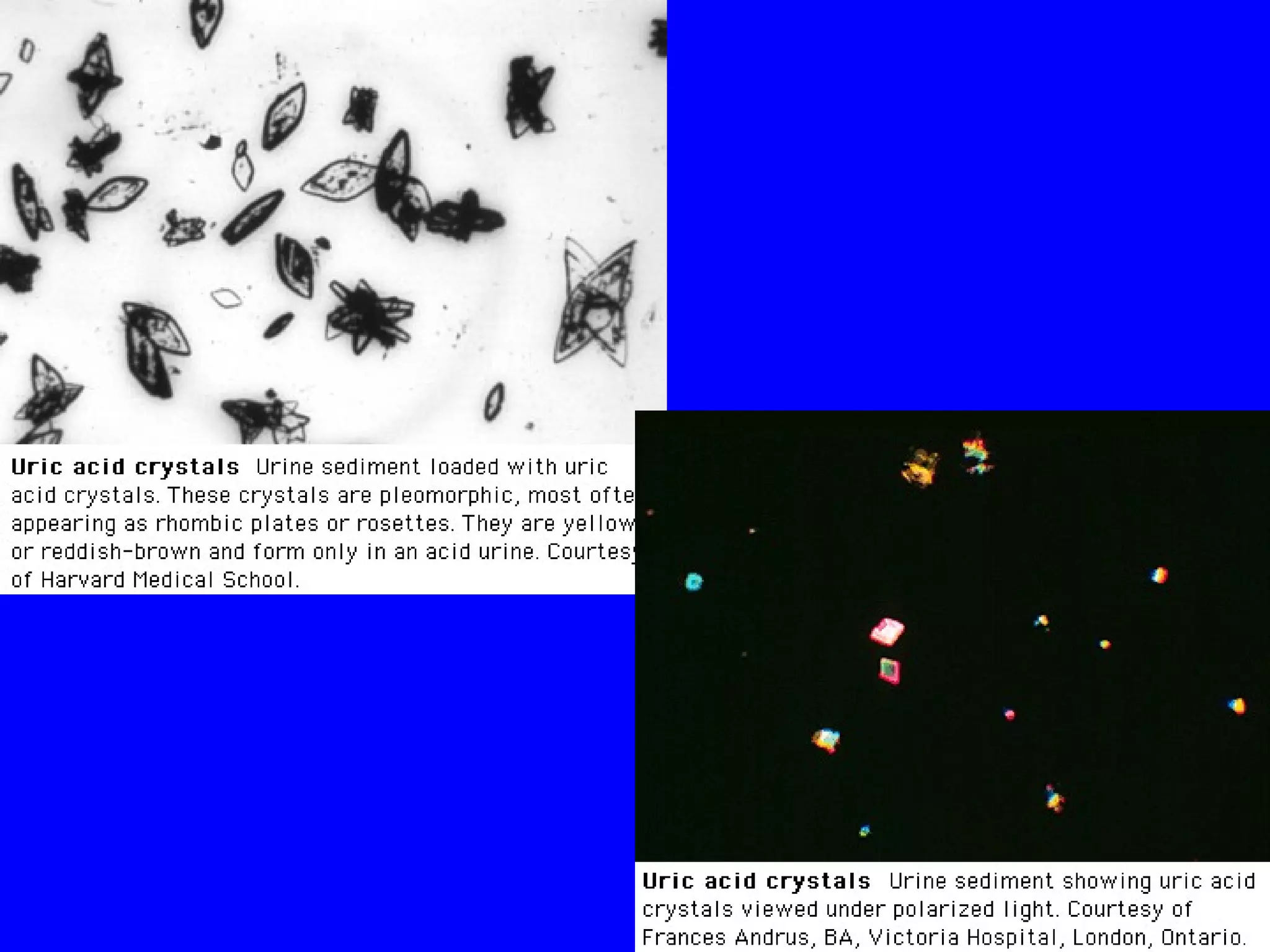
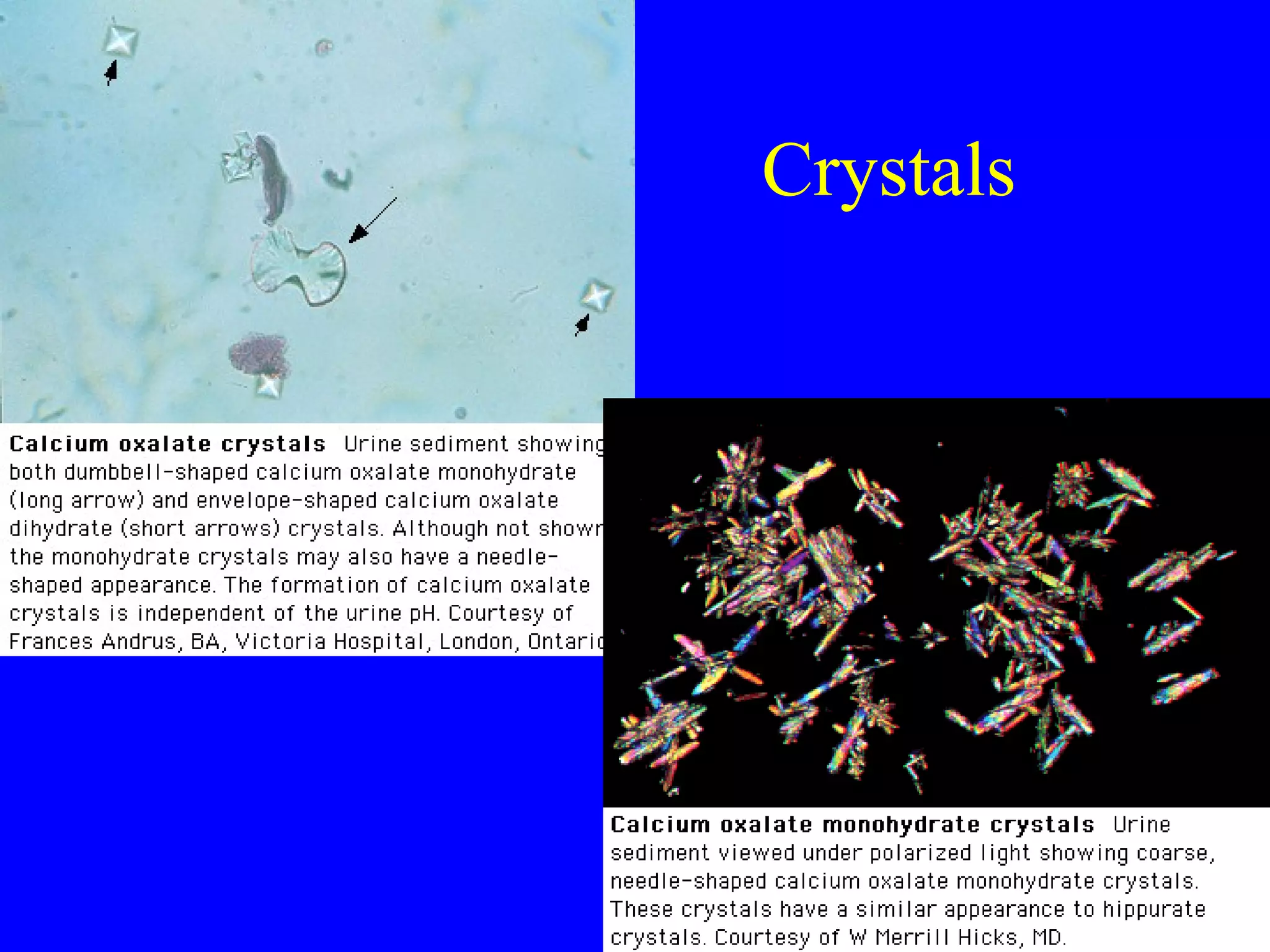
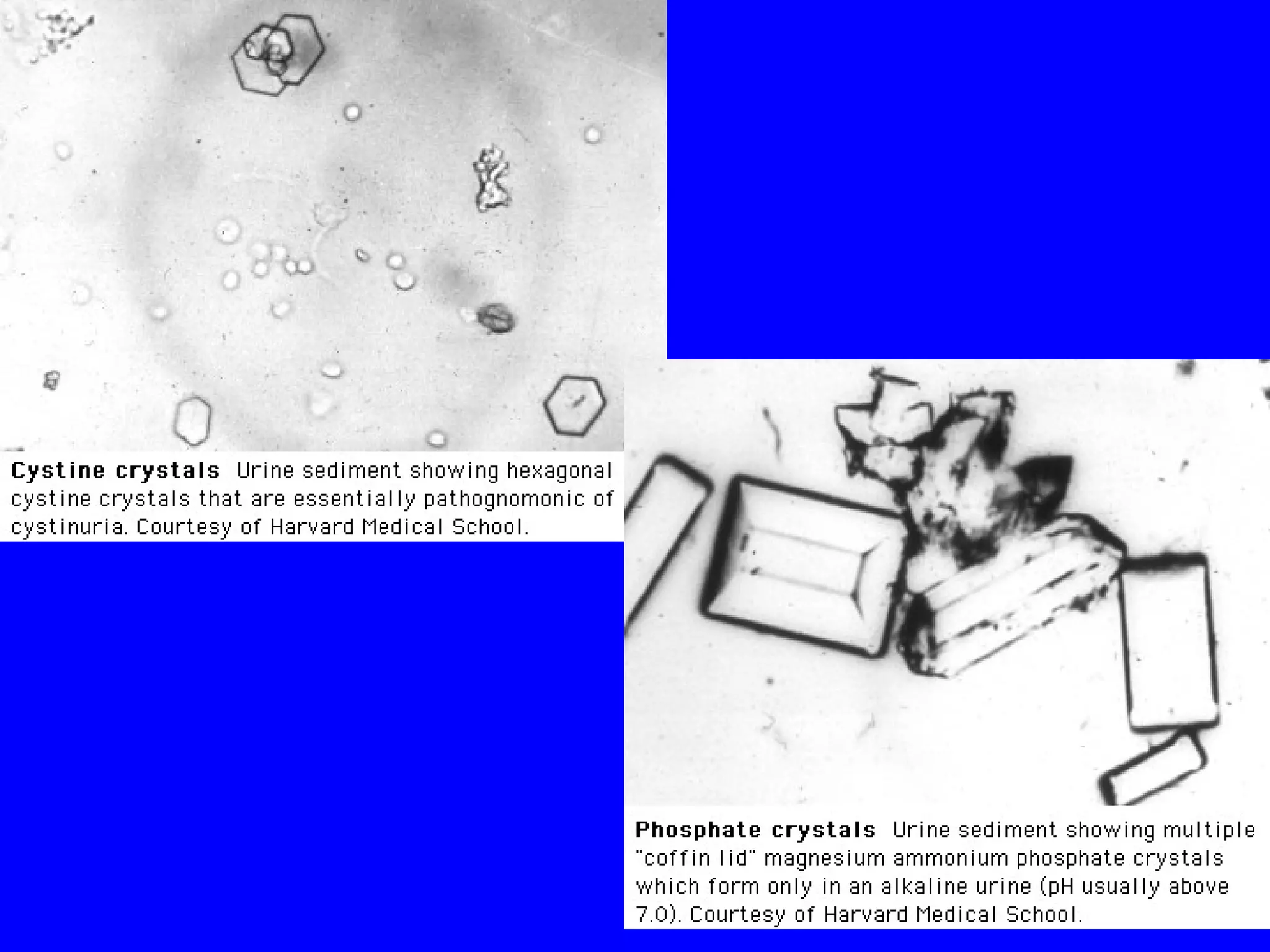
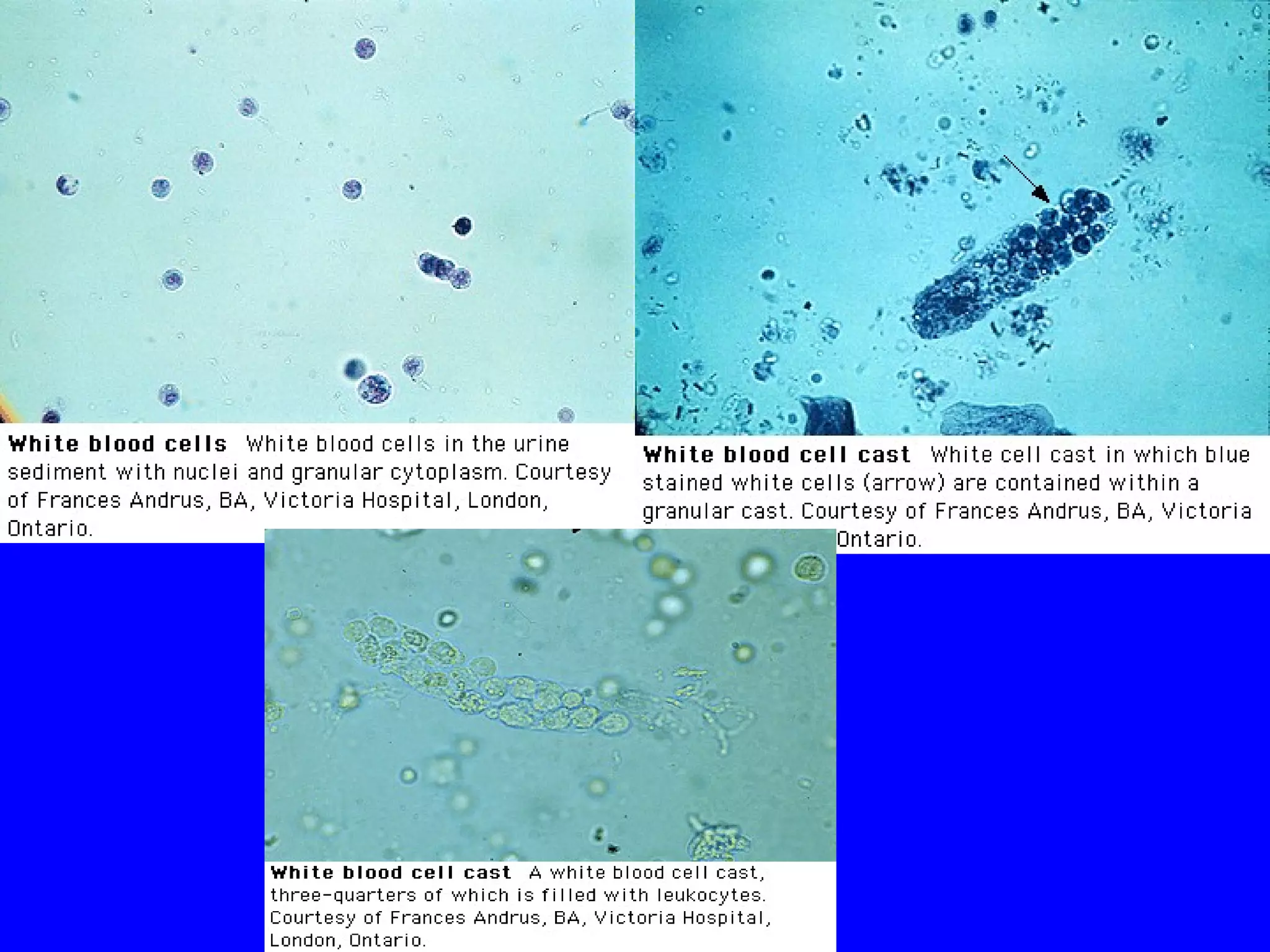
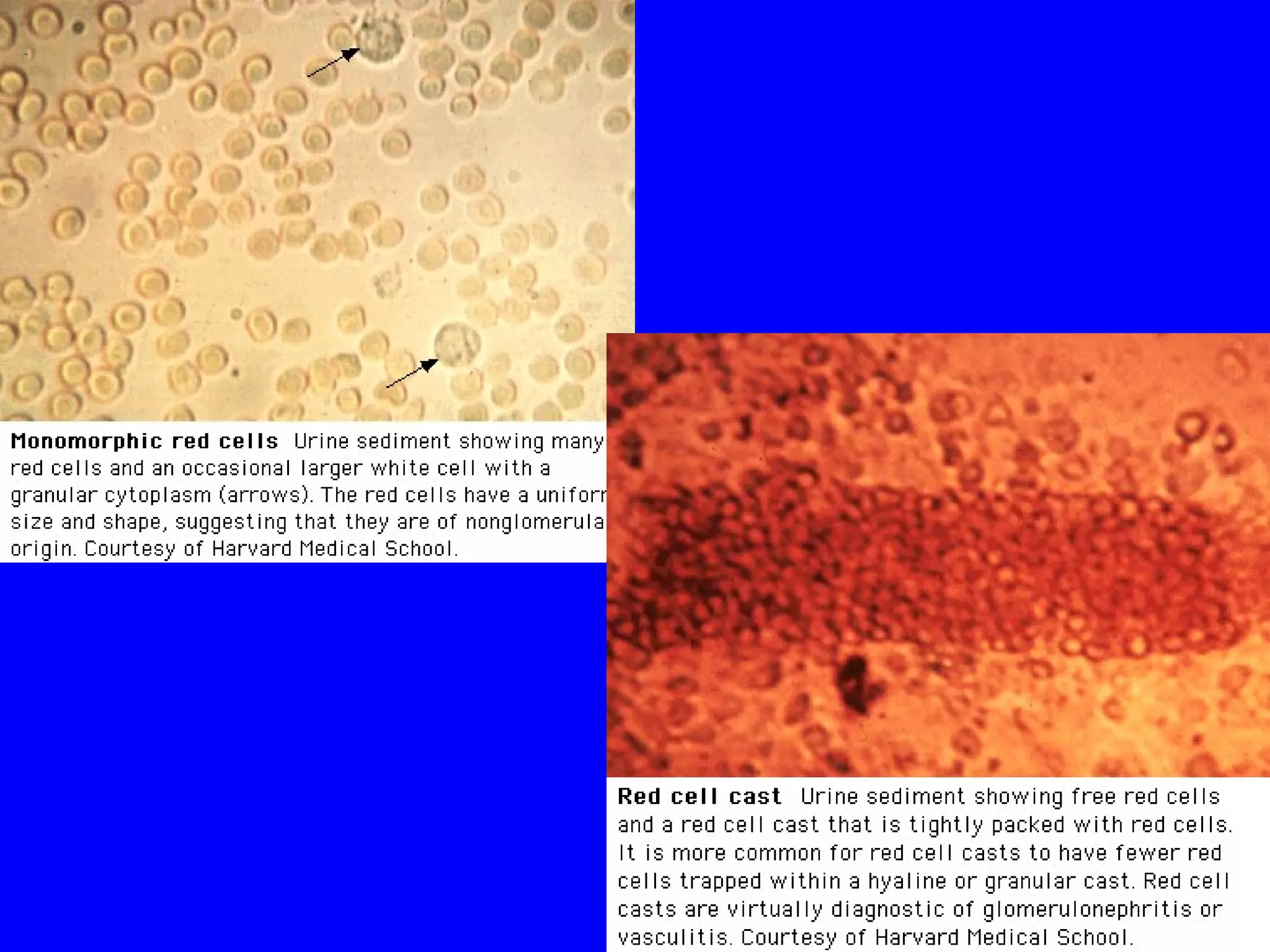
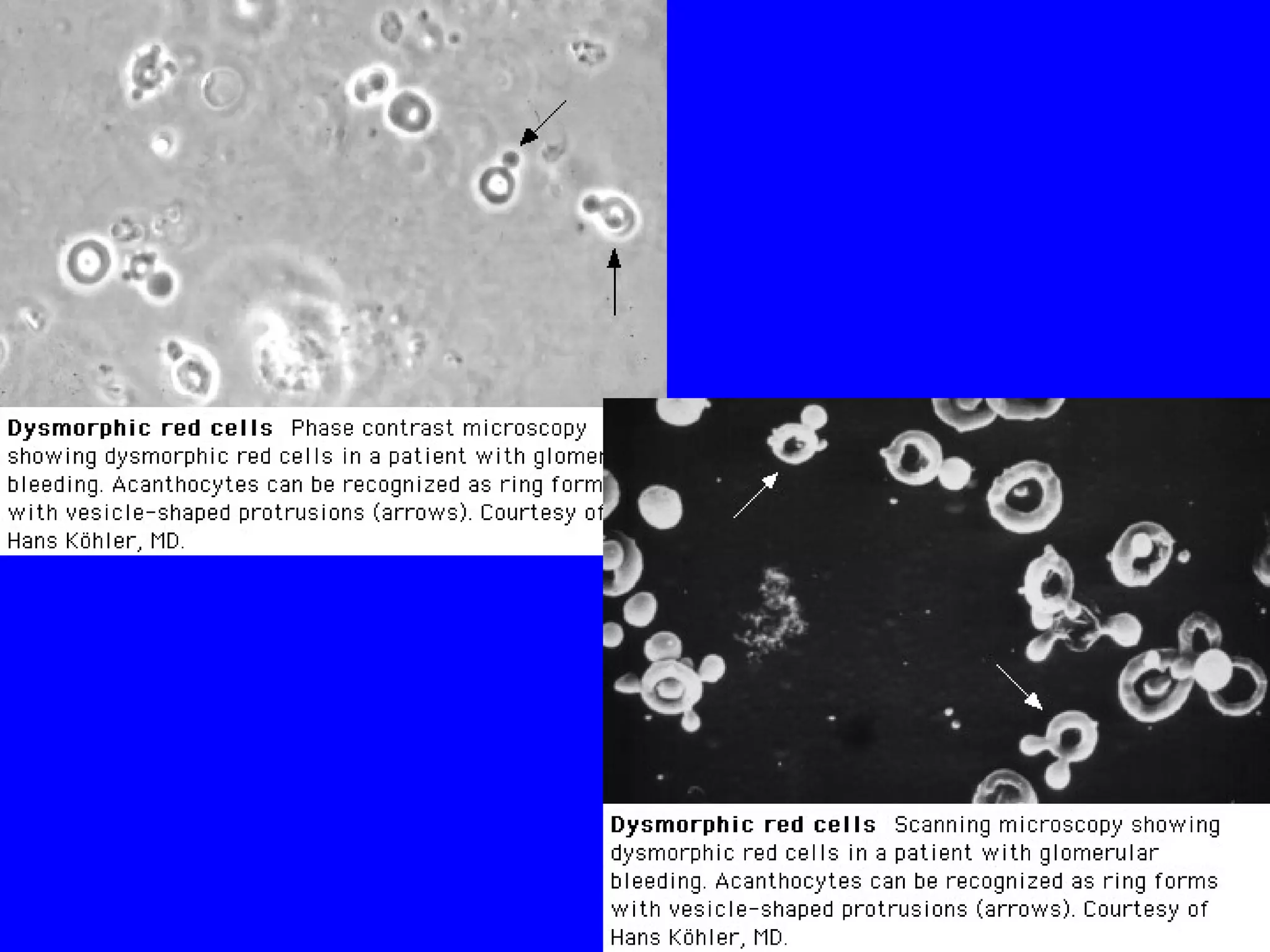
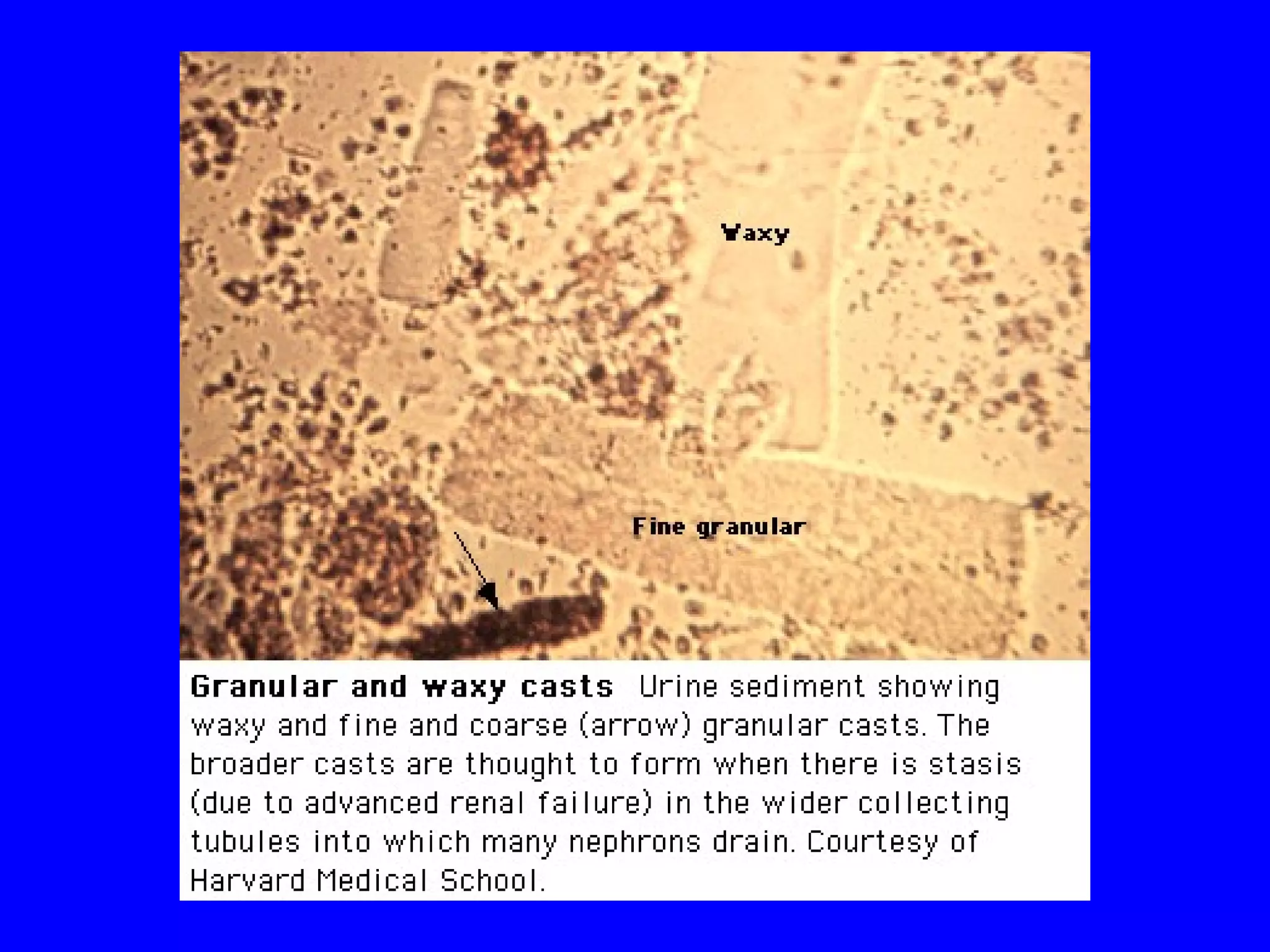
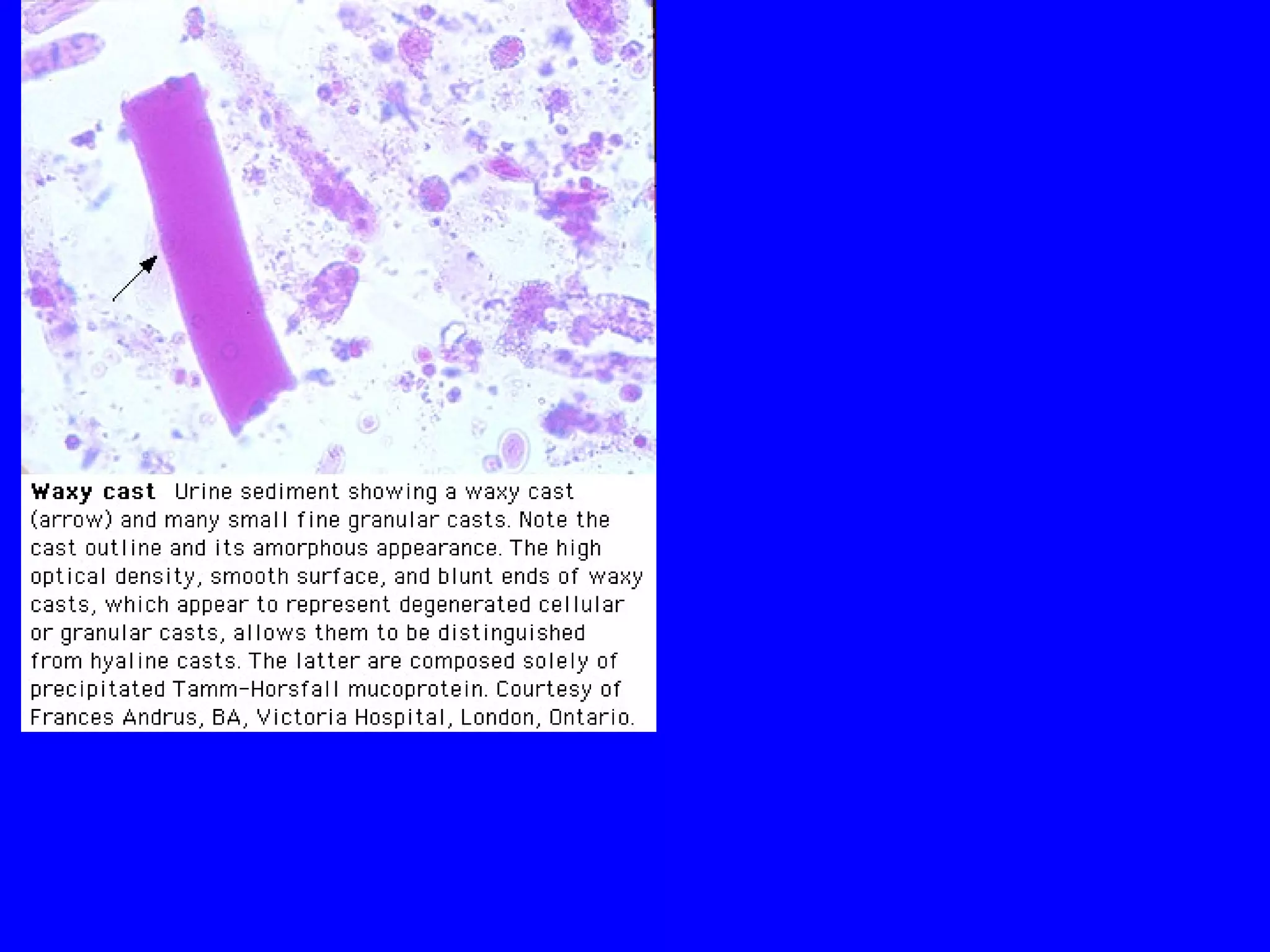
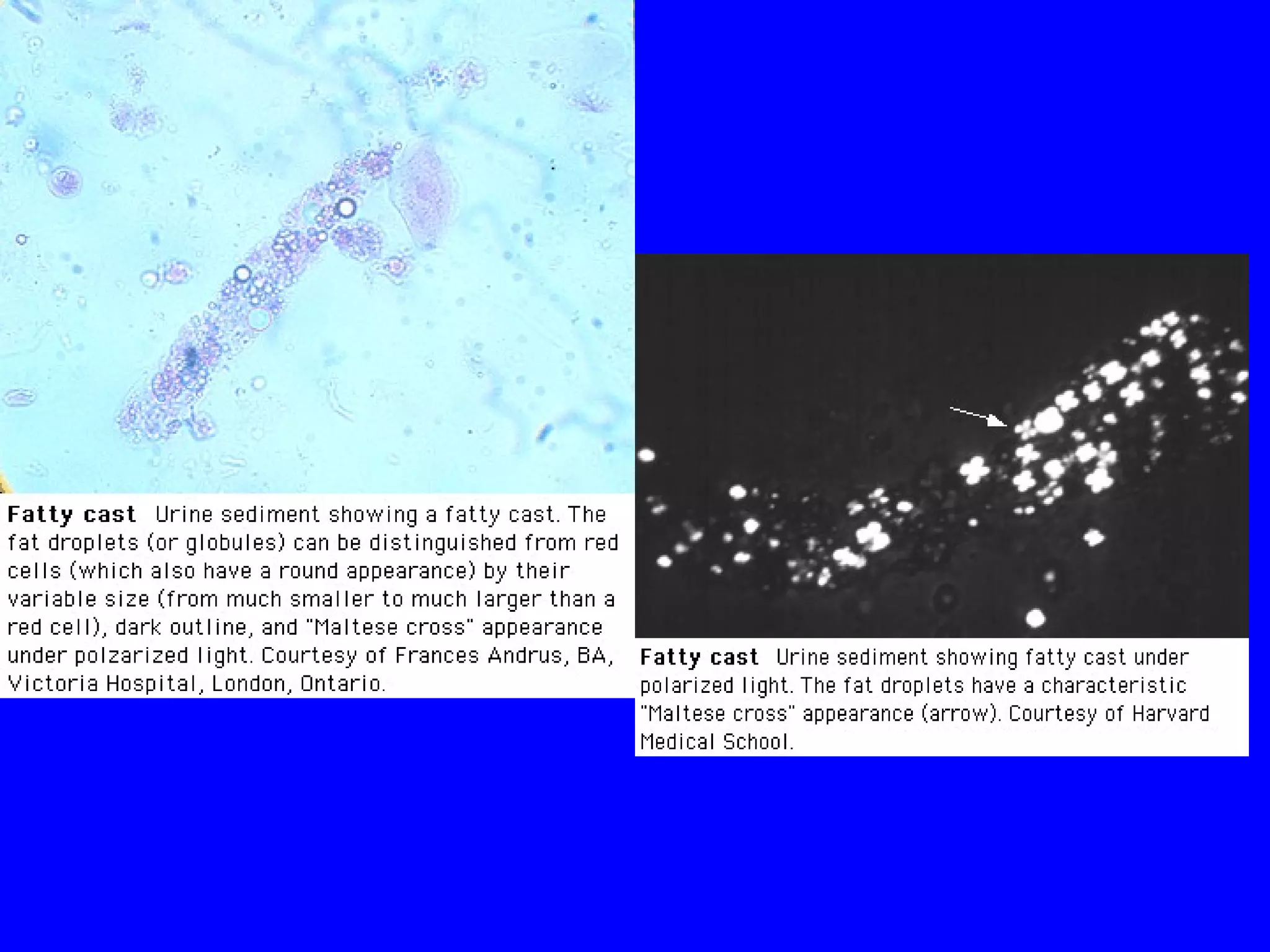
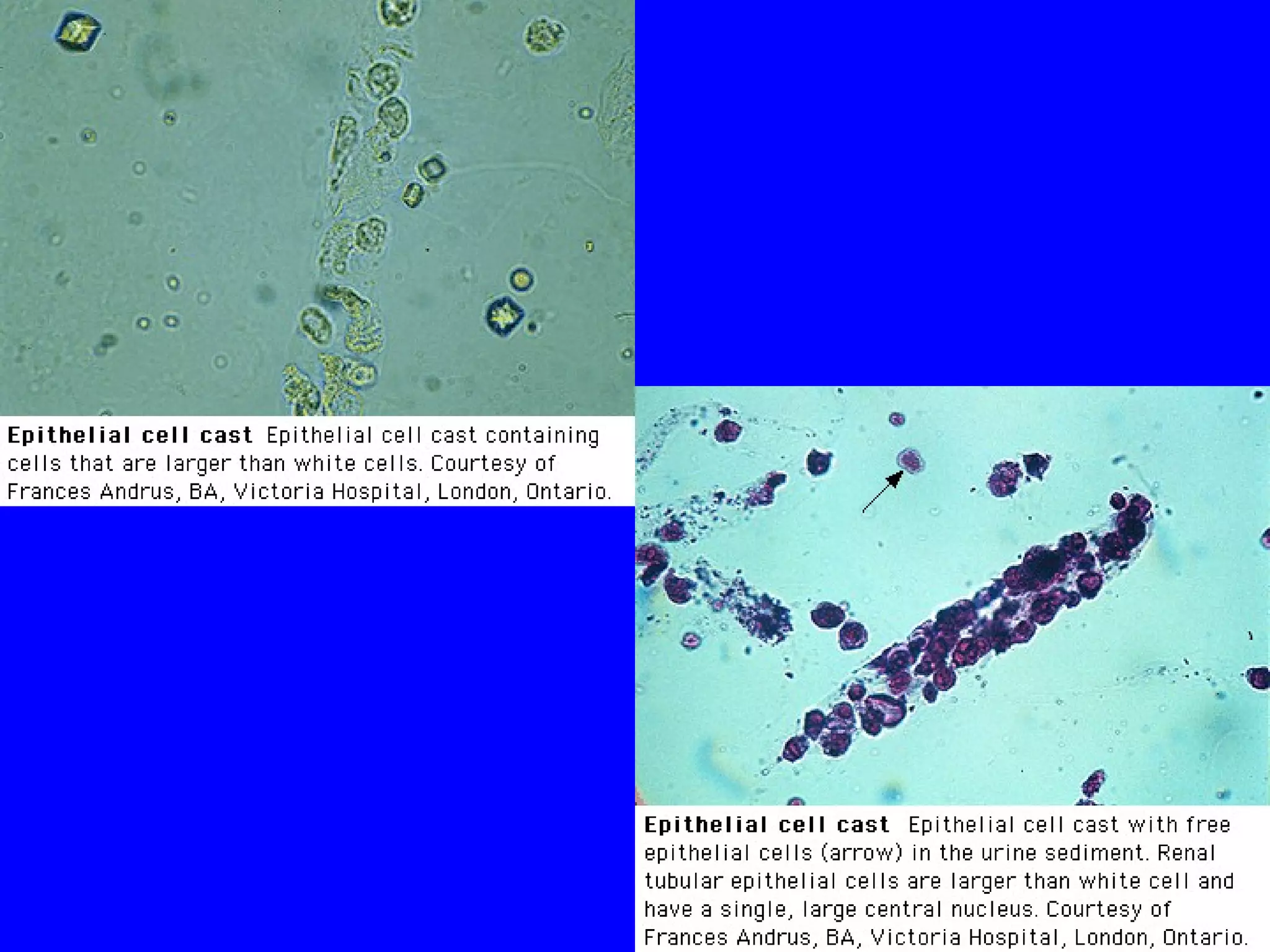
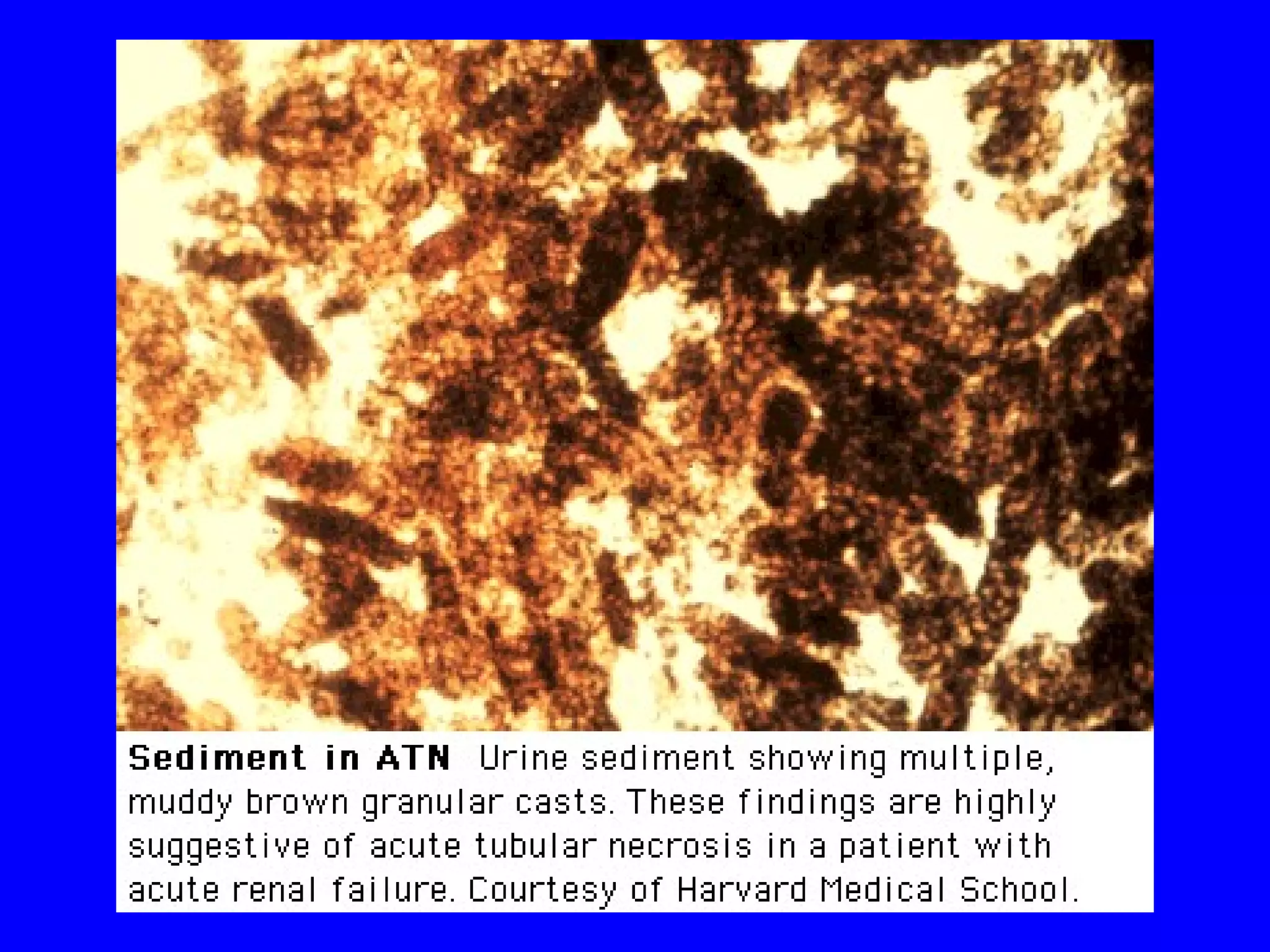
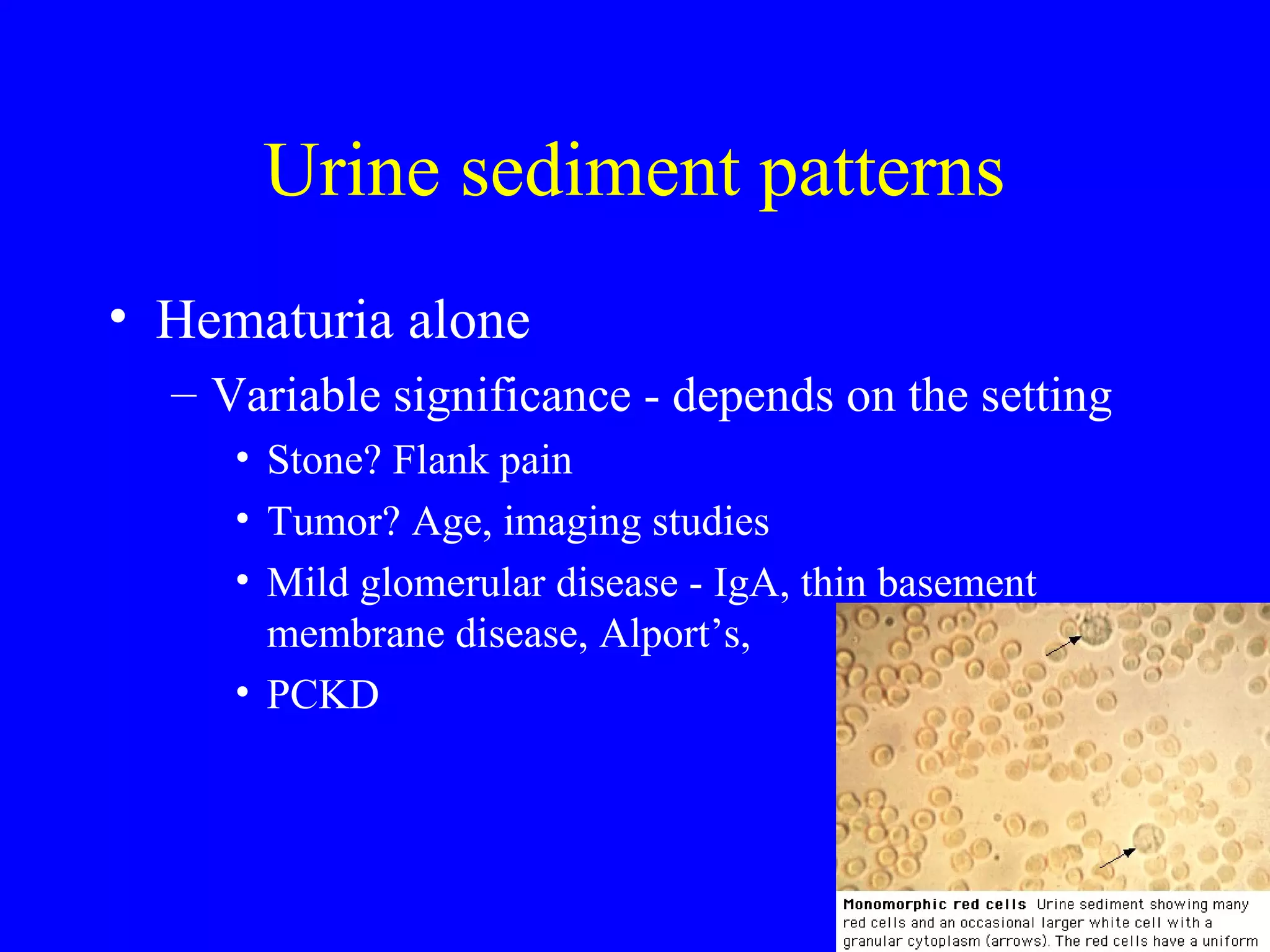
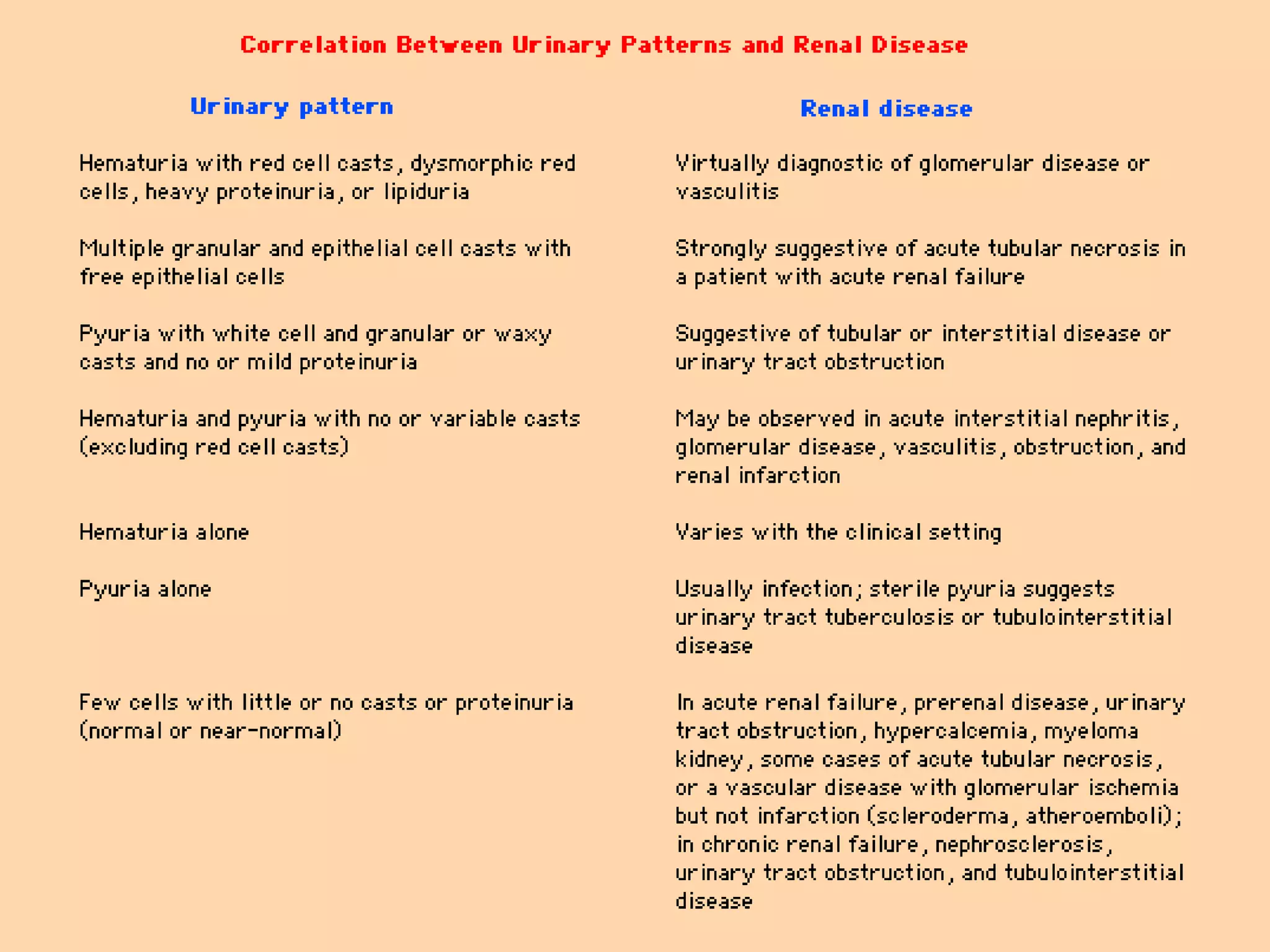
This document discusses tests used to evaluate renal function, including estimates of glomerular filtration rate (GFR) using serum creatinine, BUN, eGFR formulas, and creatinine clearance tests. It describes the production and handling of creatinine by the kidneys and limitations of eGFR estimates. The document also covers urinalysis components like urine color, specific gravity, protein, and sediment analysis and what various findings indicate about kidney conditions.