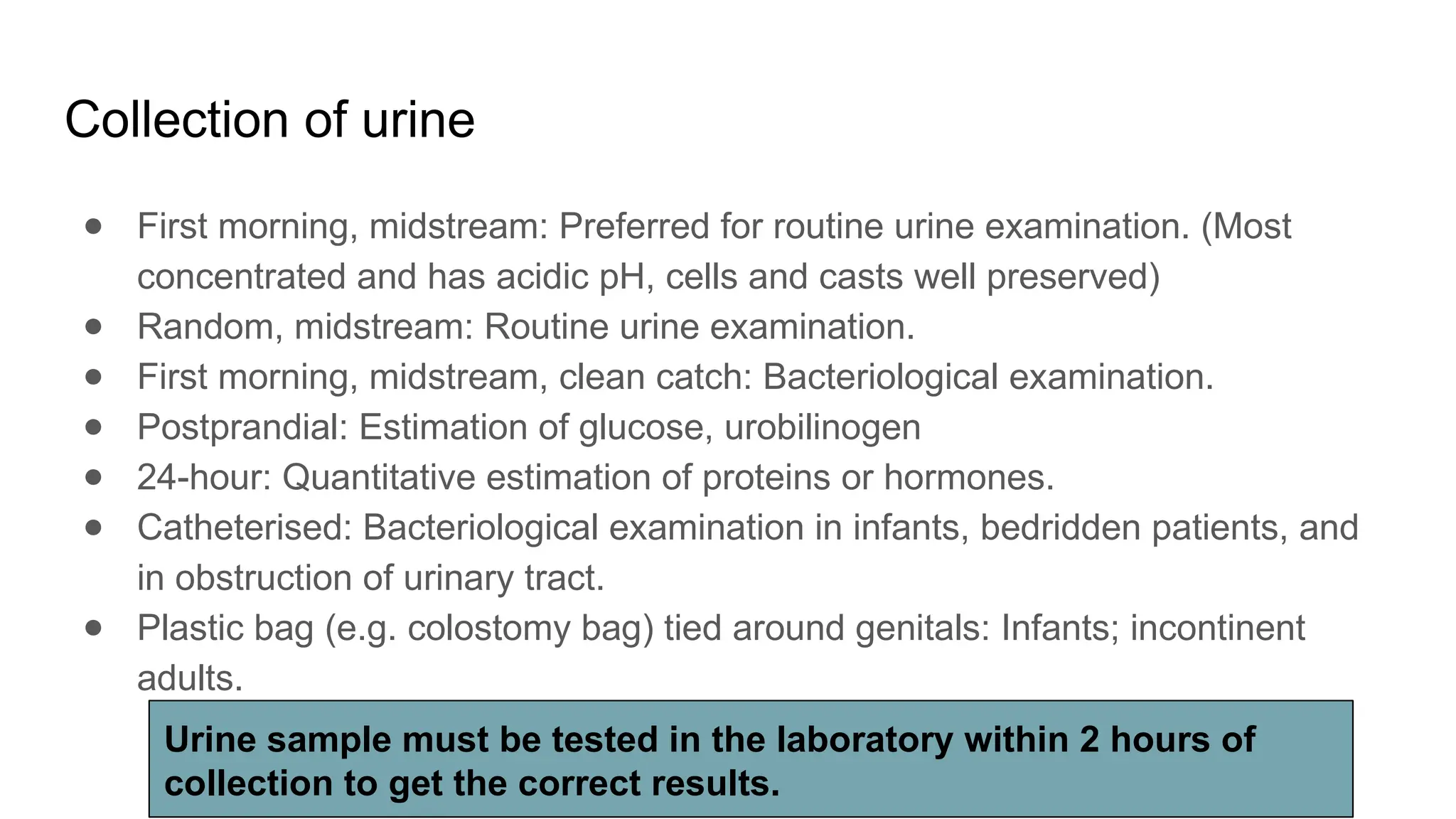
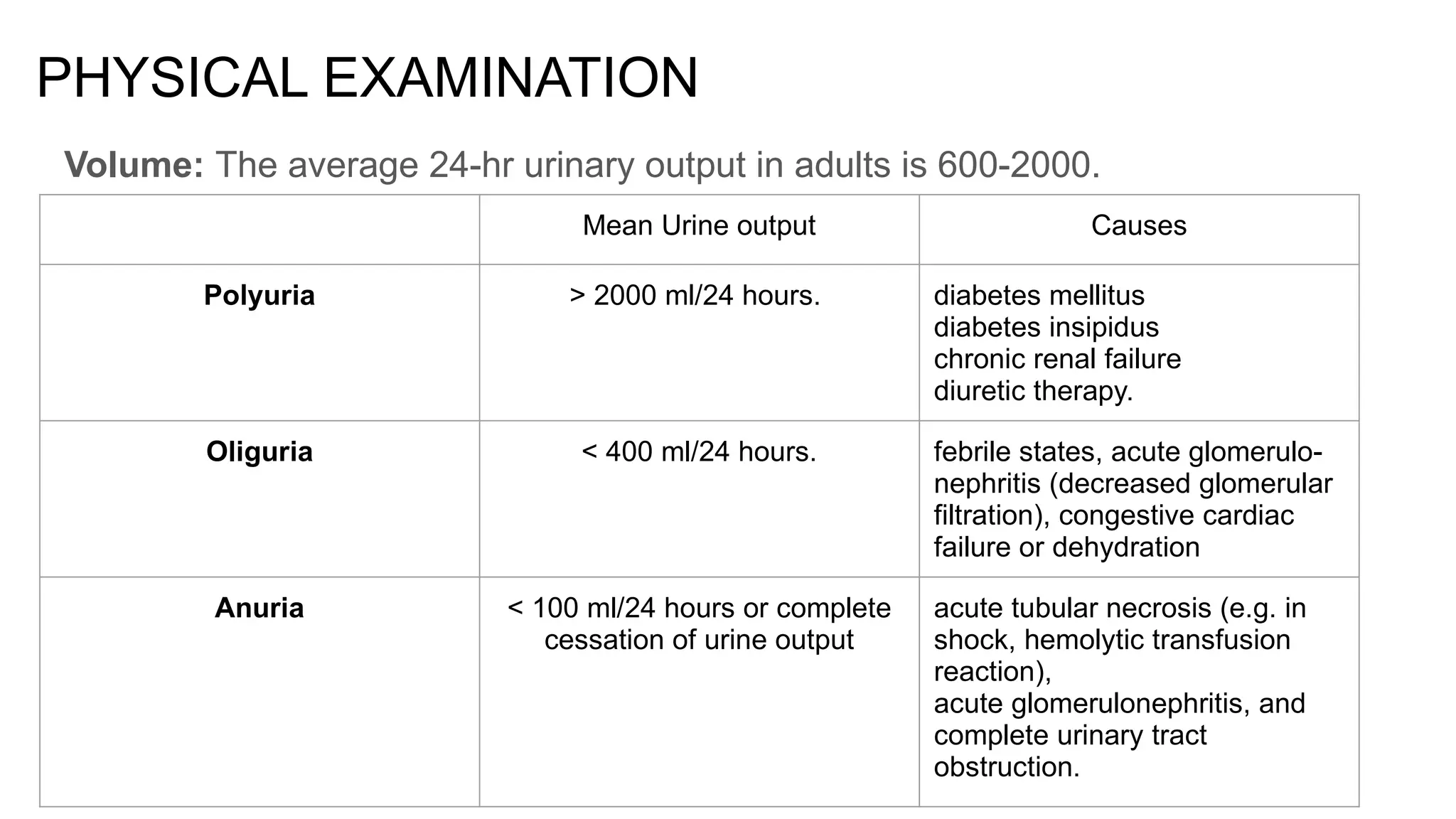
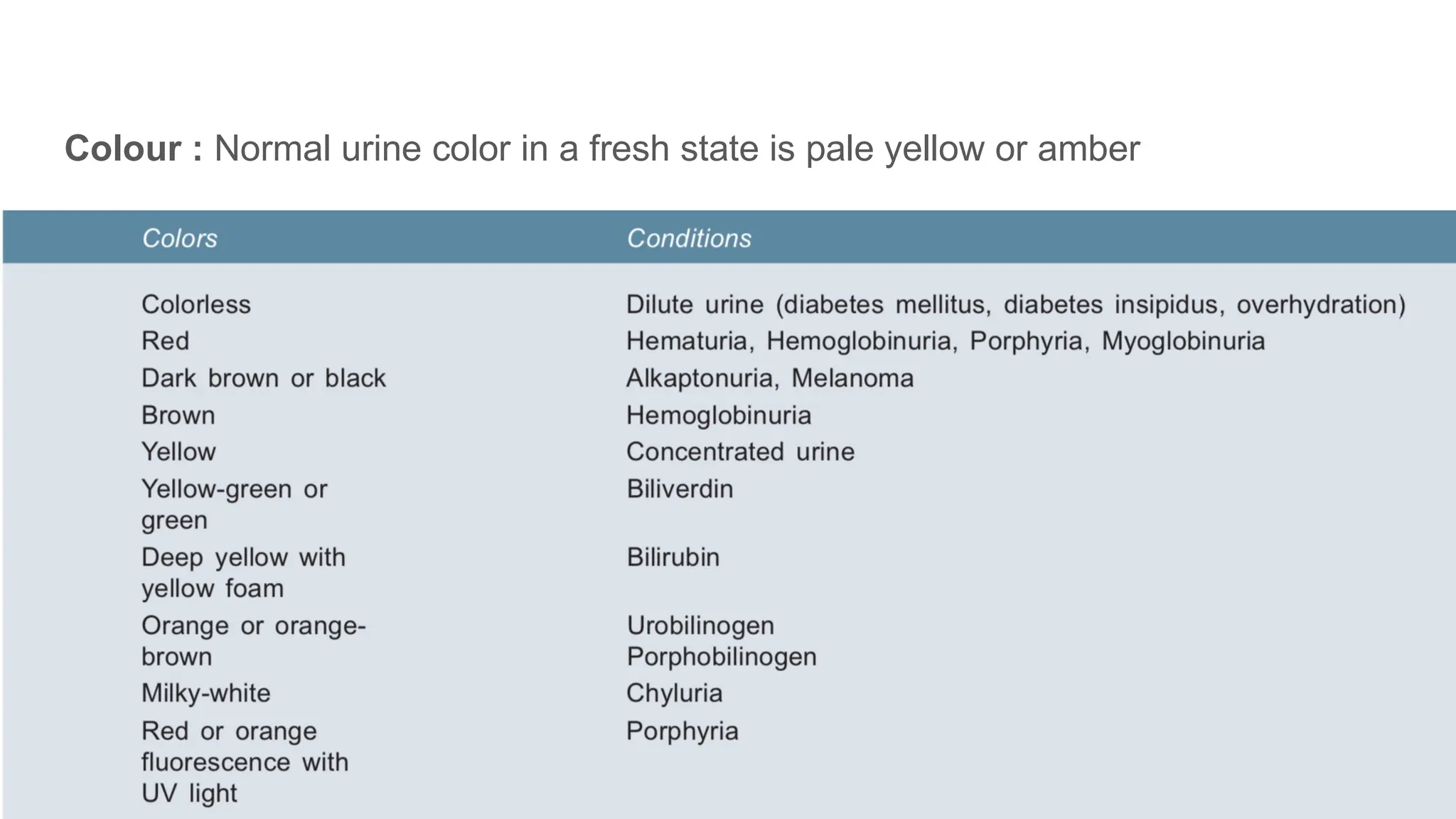
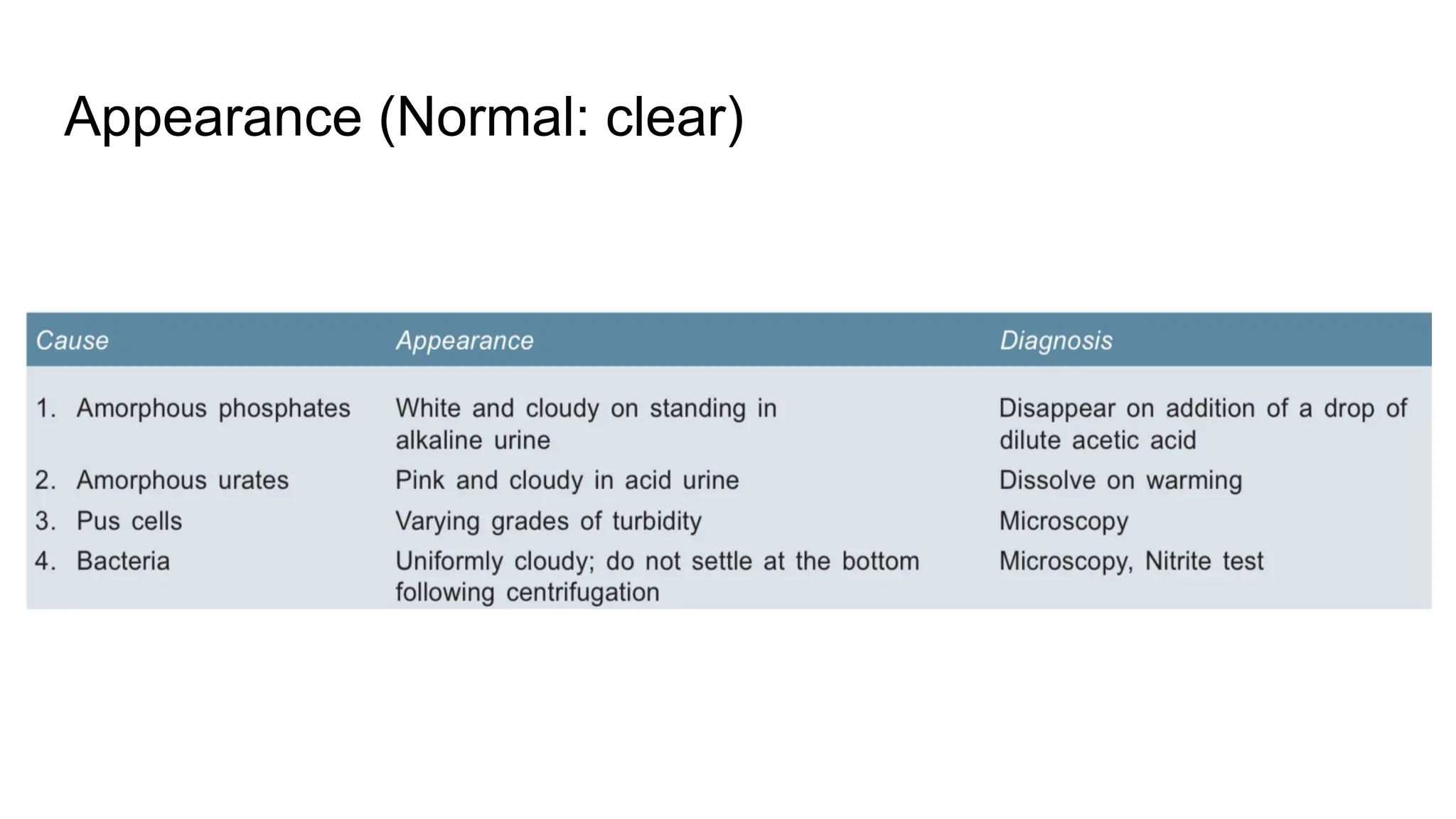
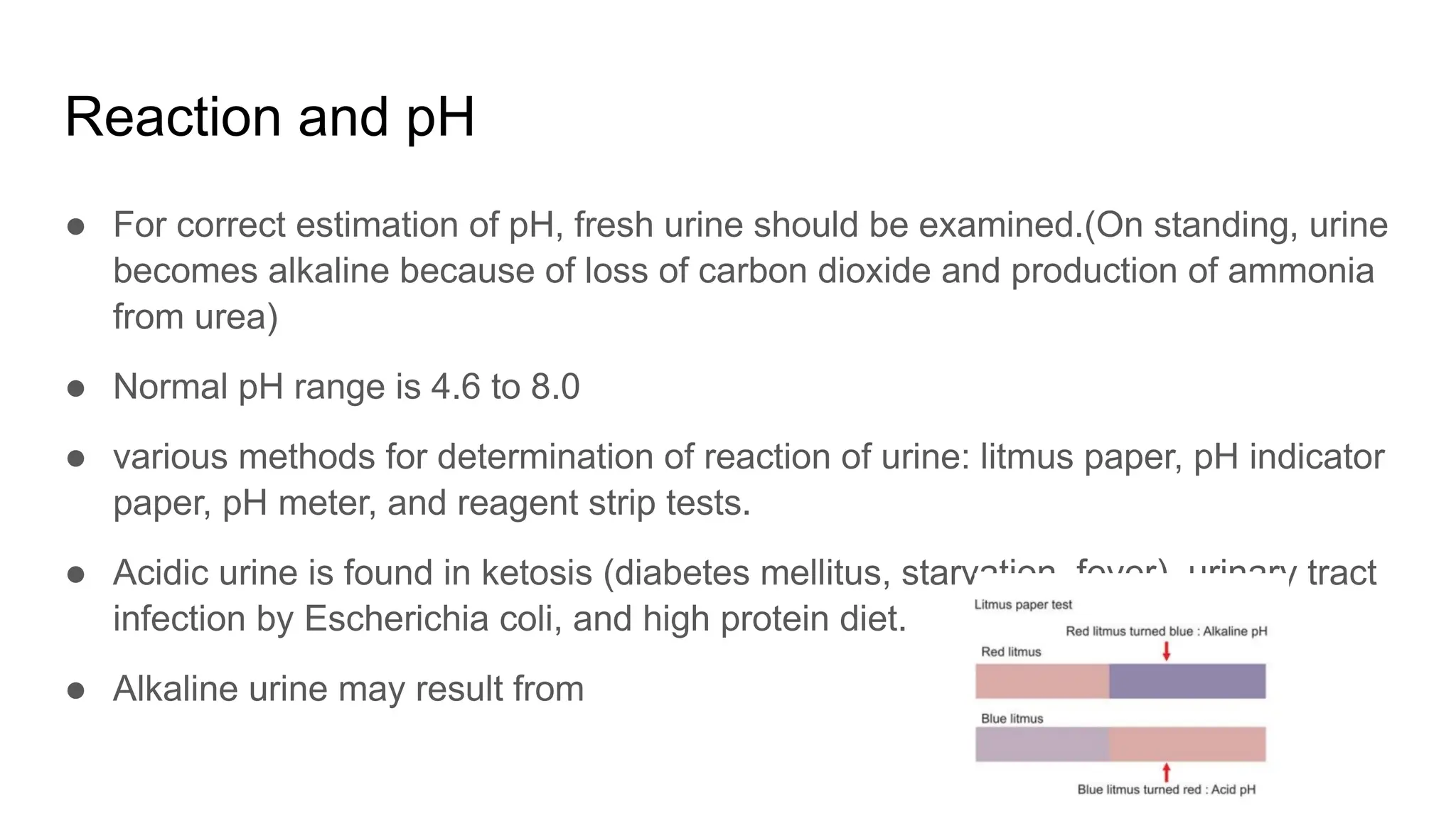
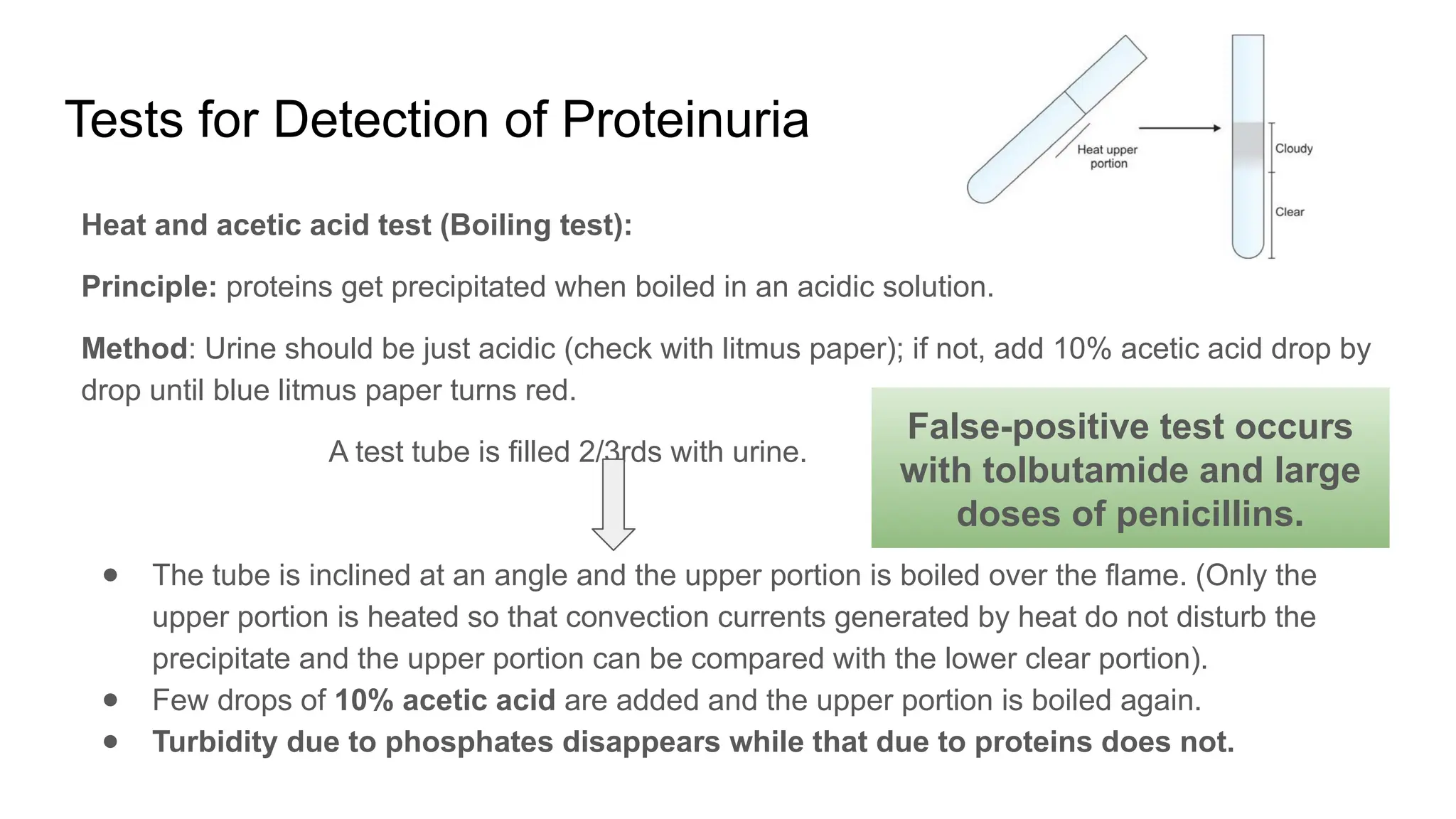
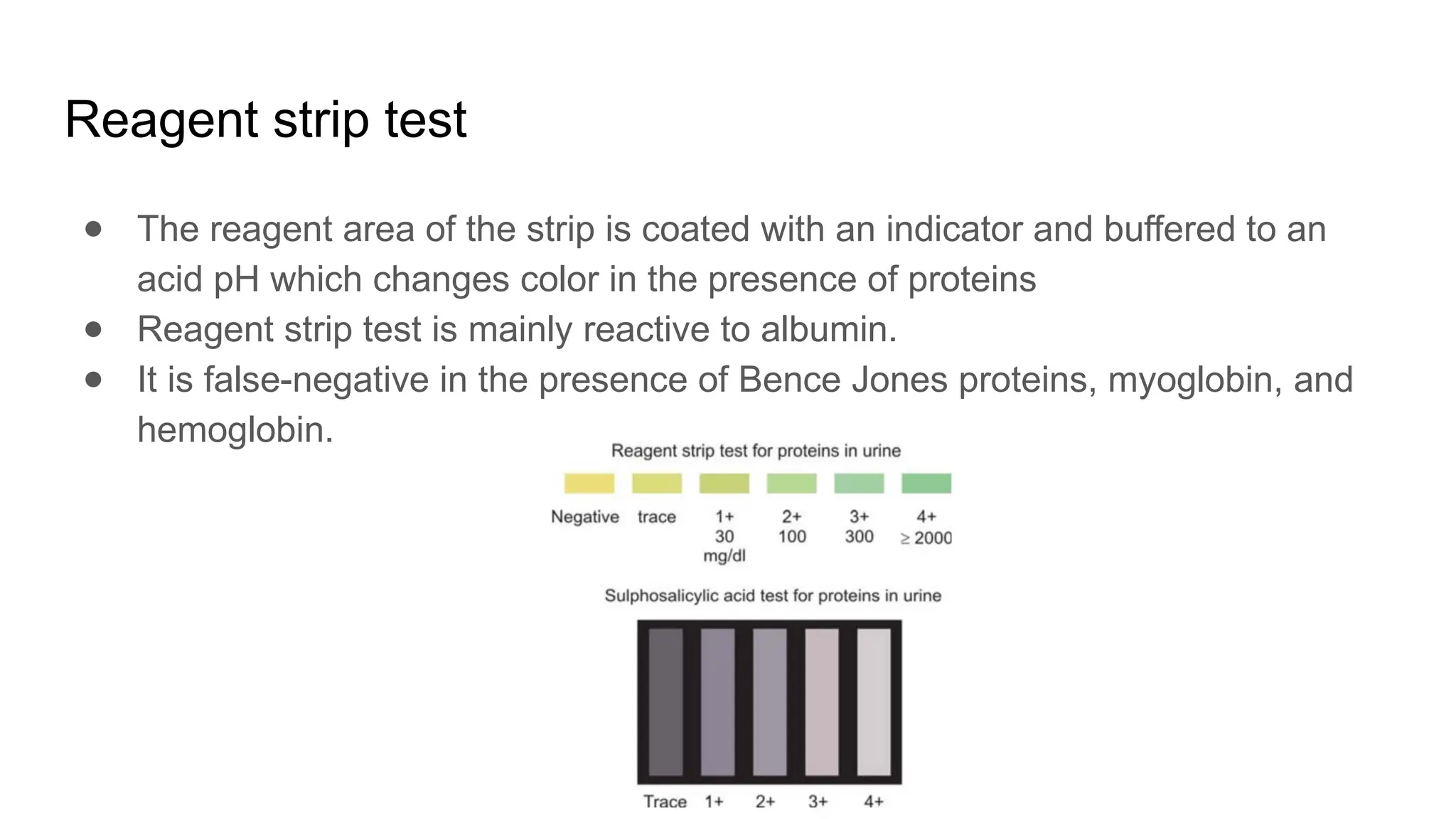
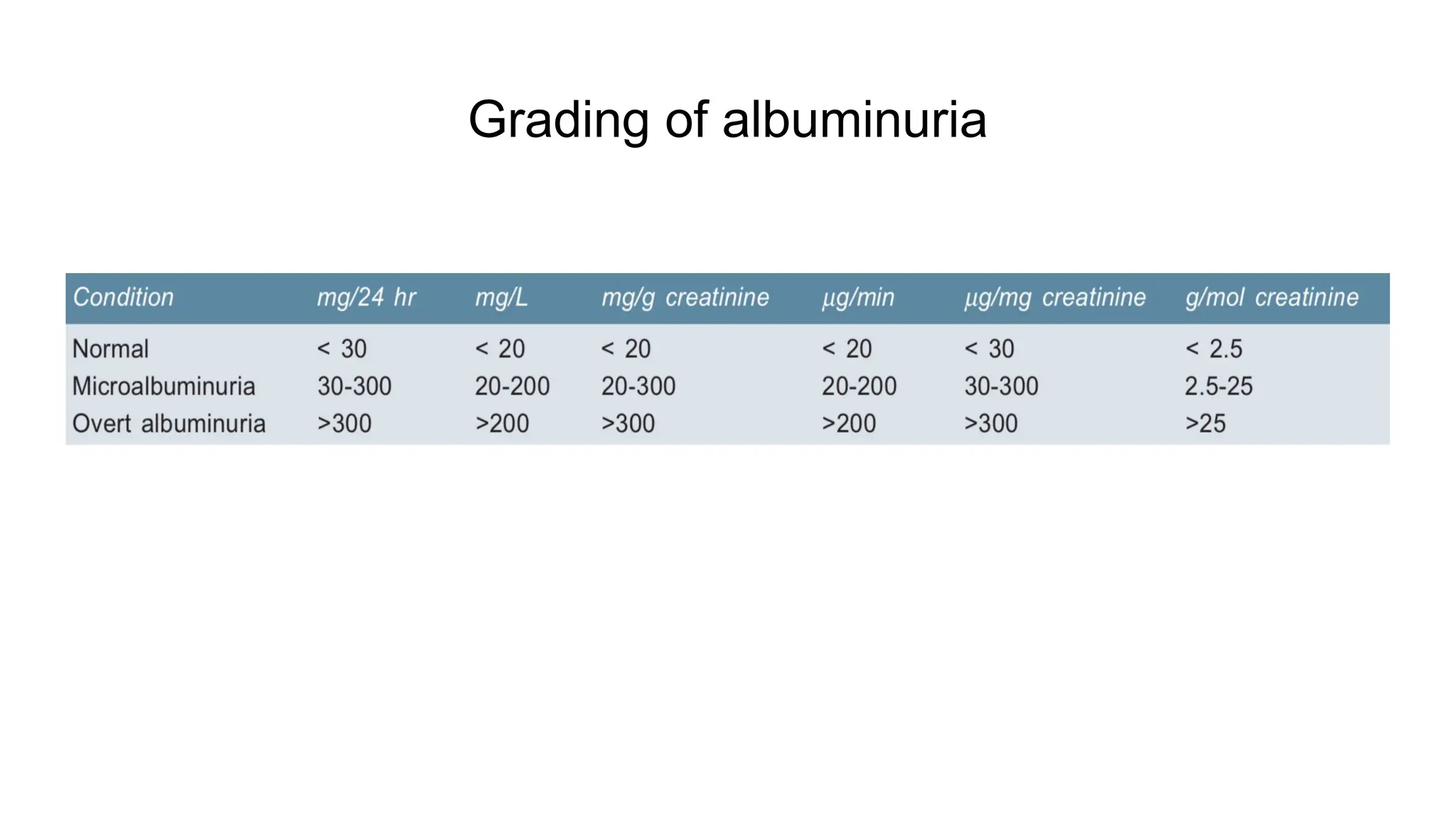
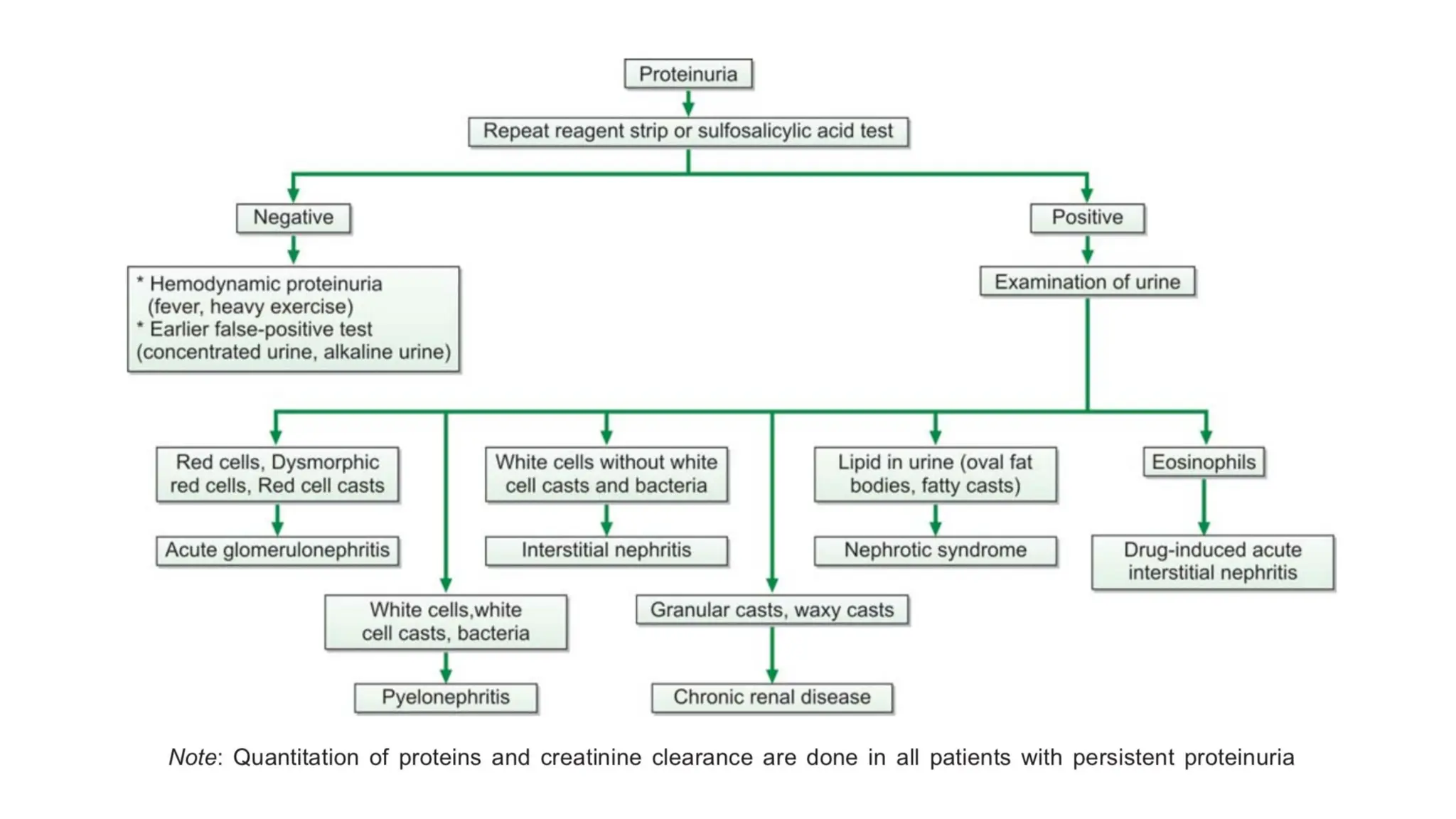
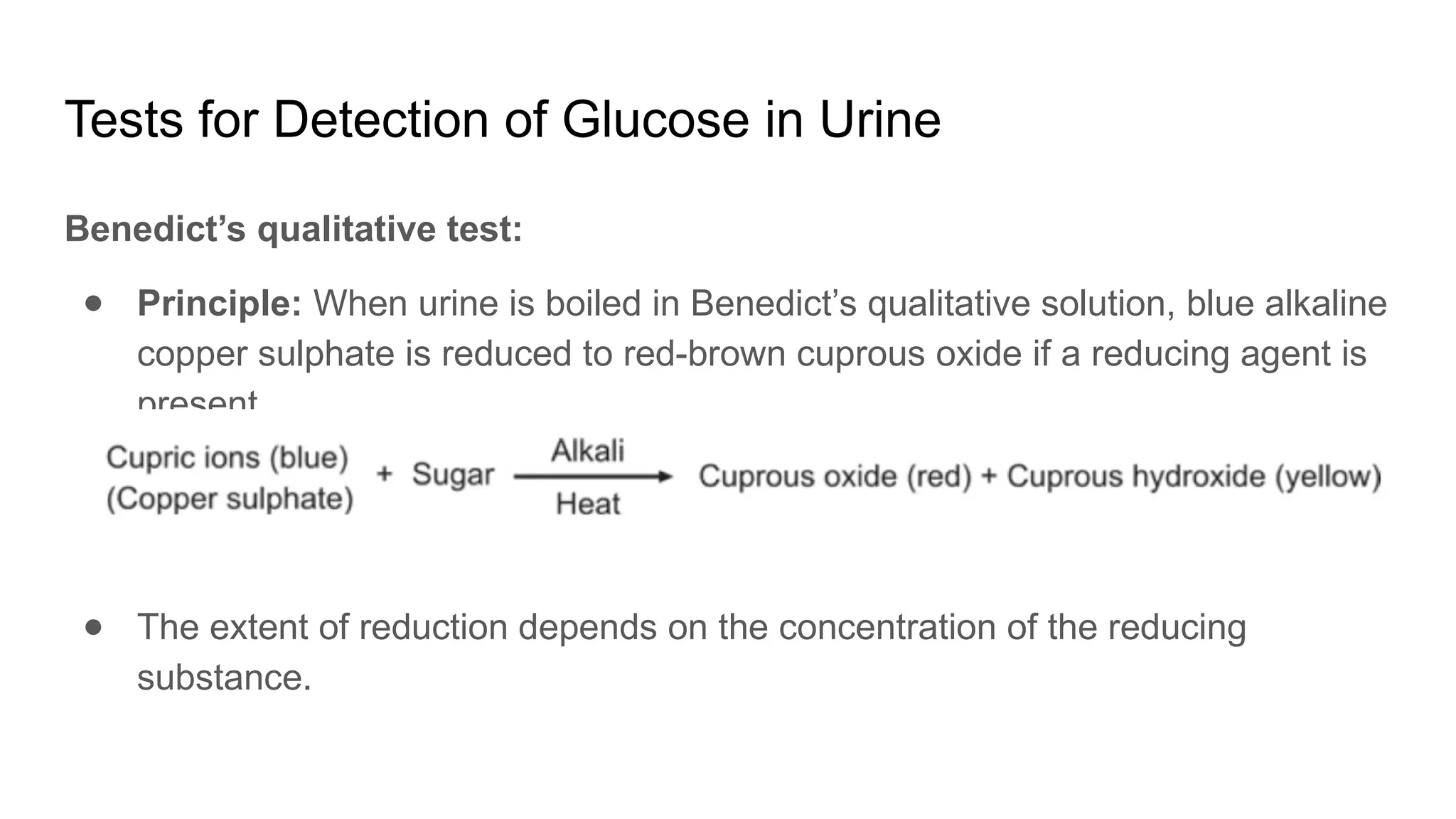
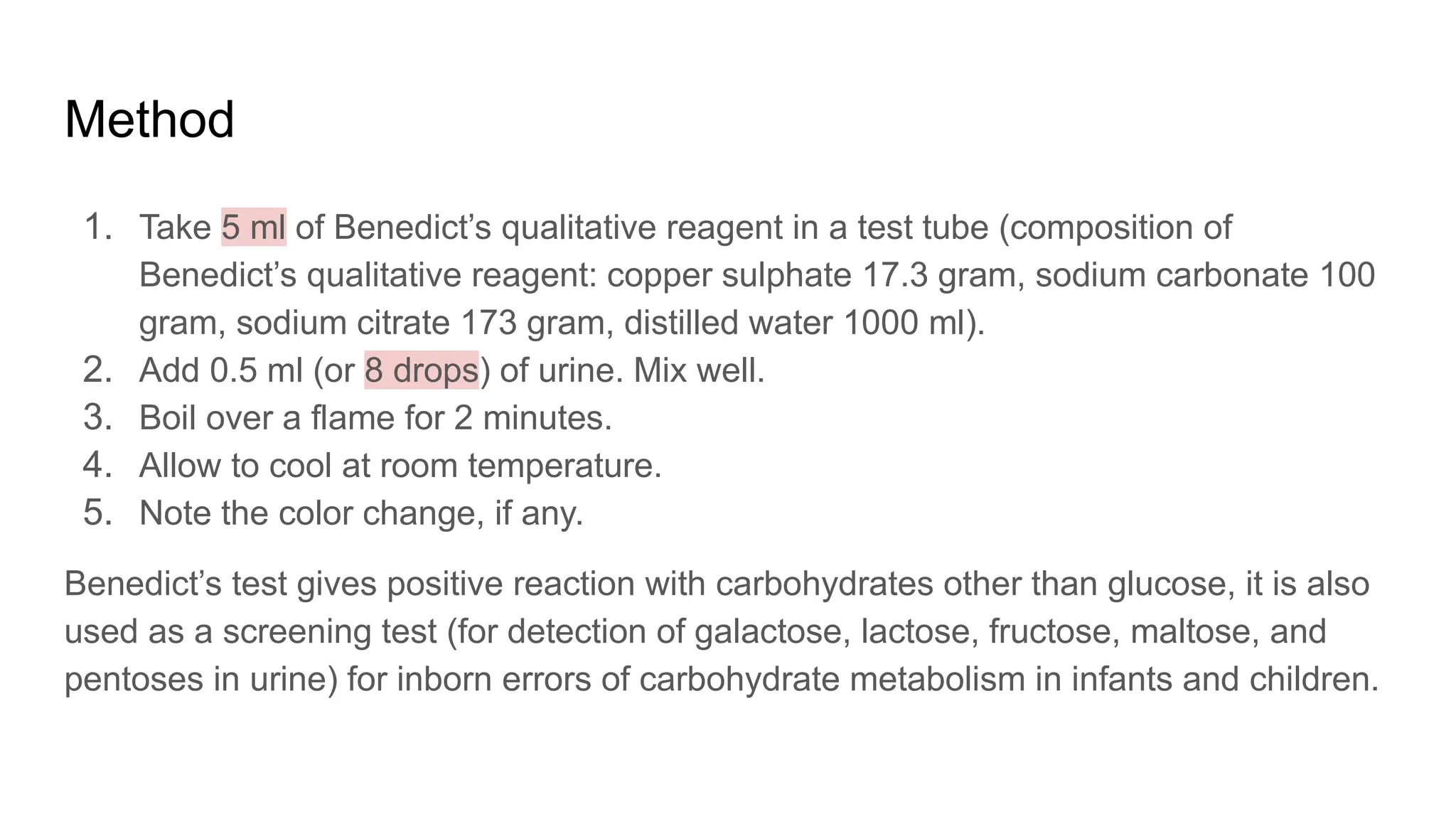
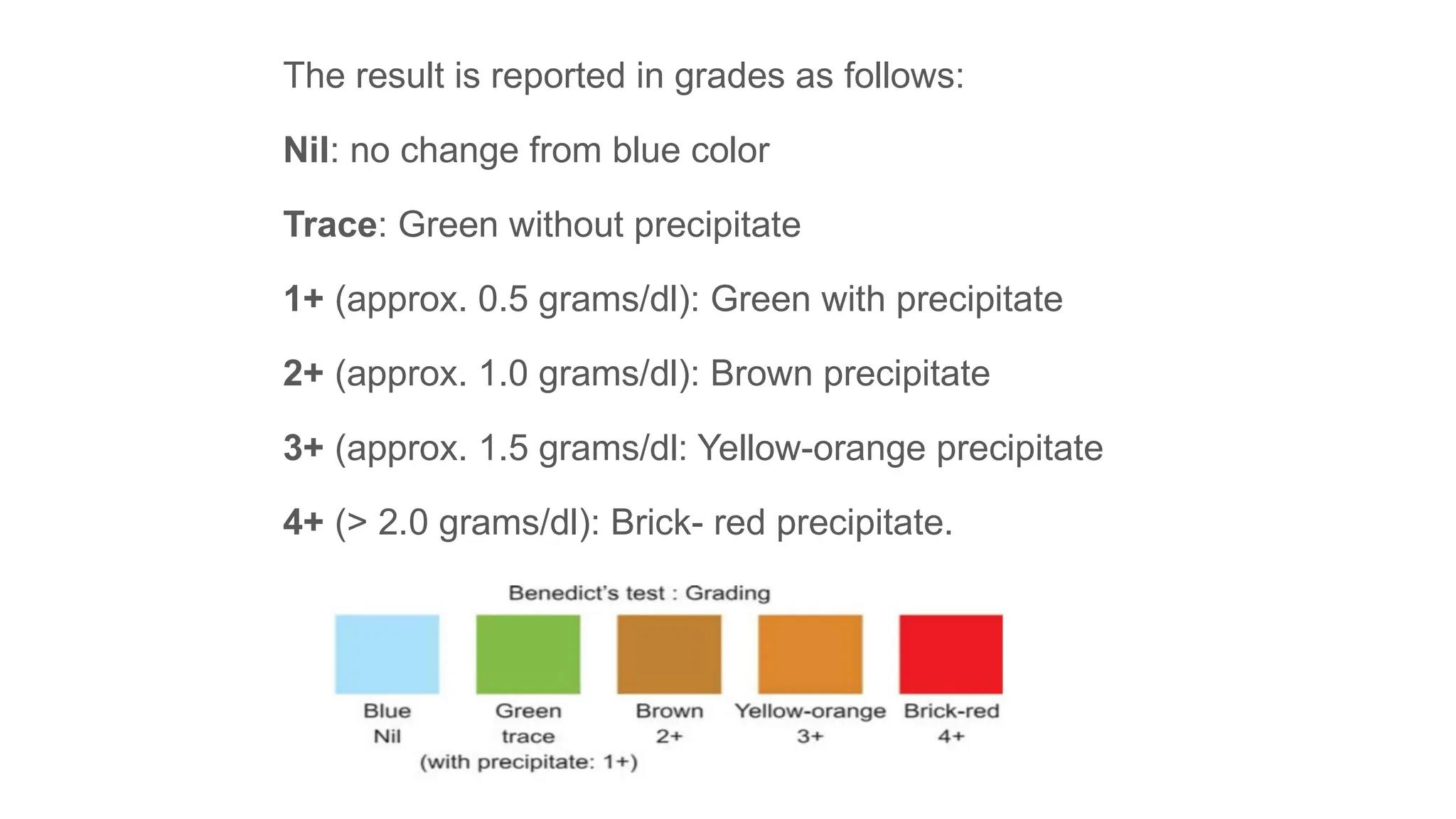
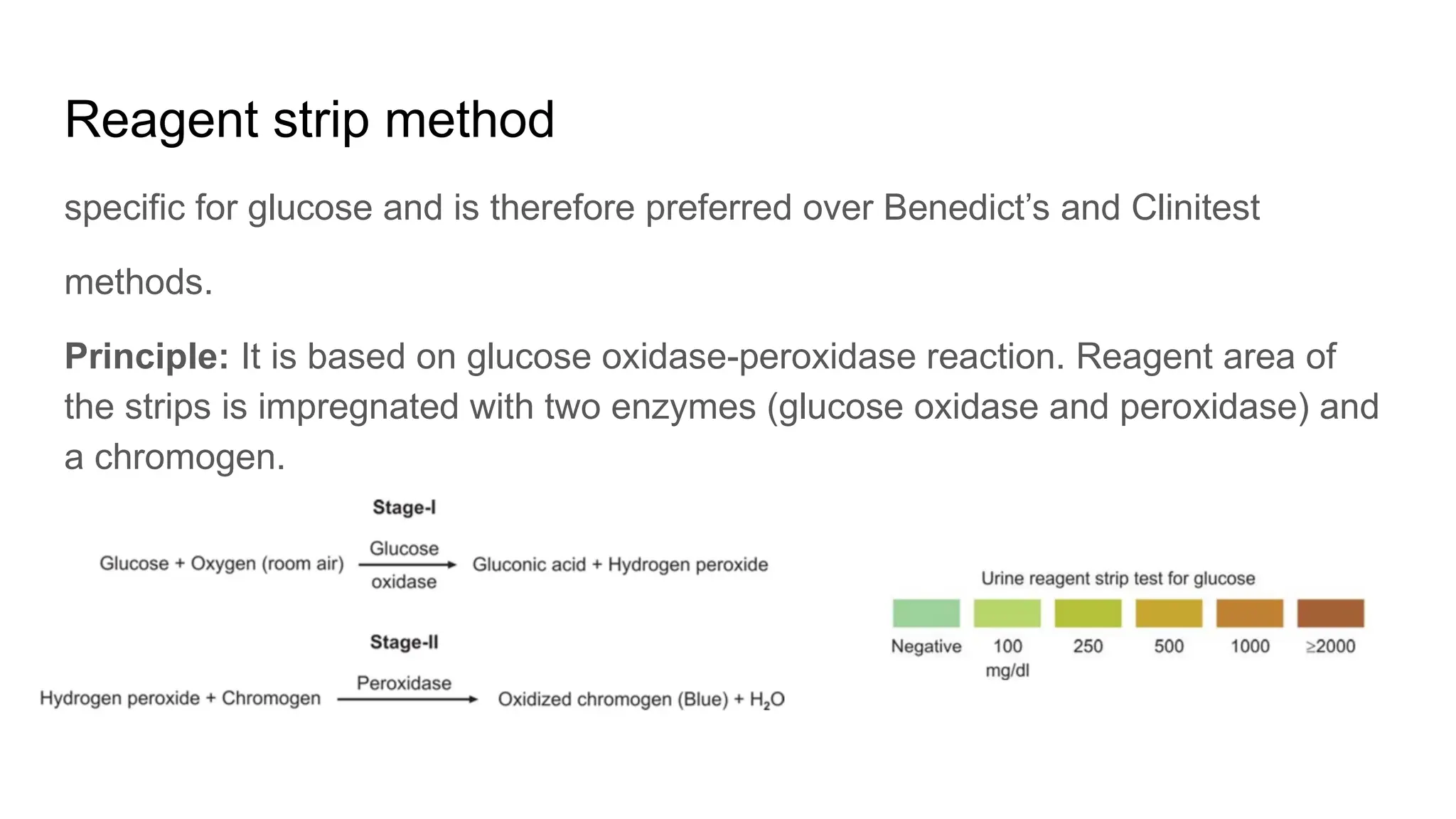
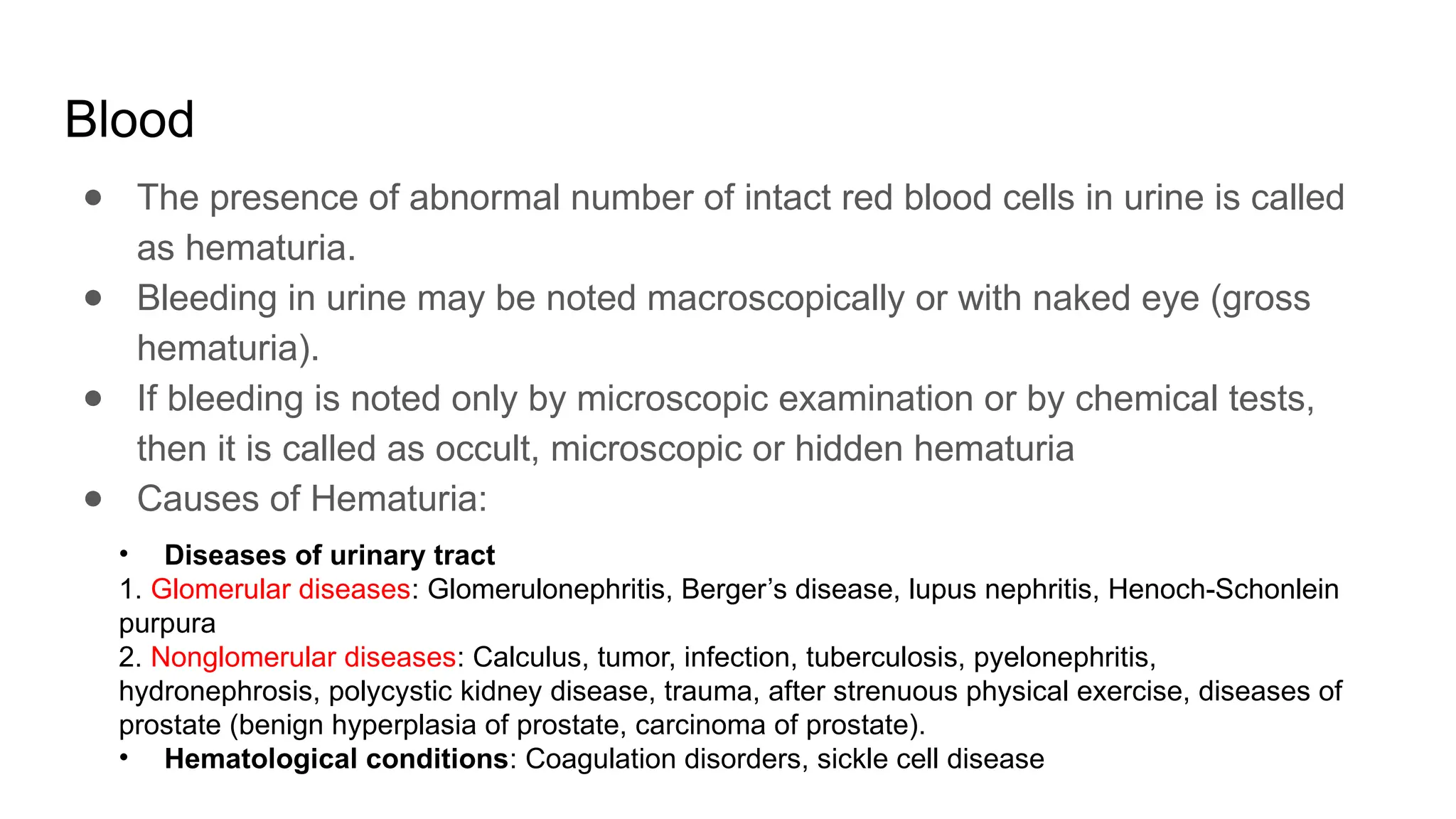
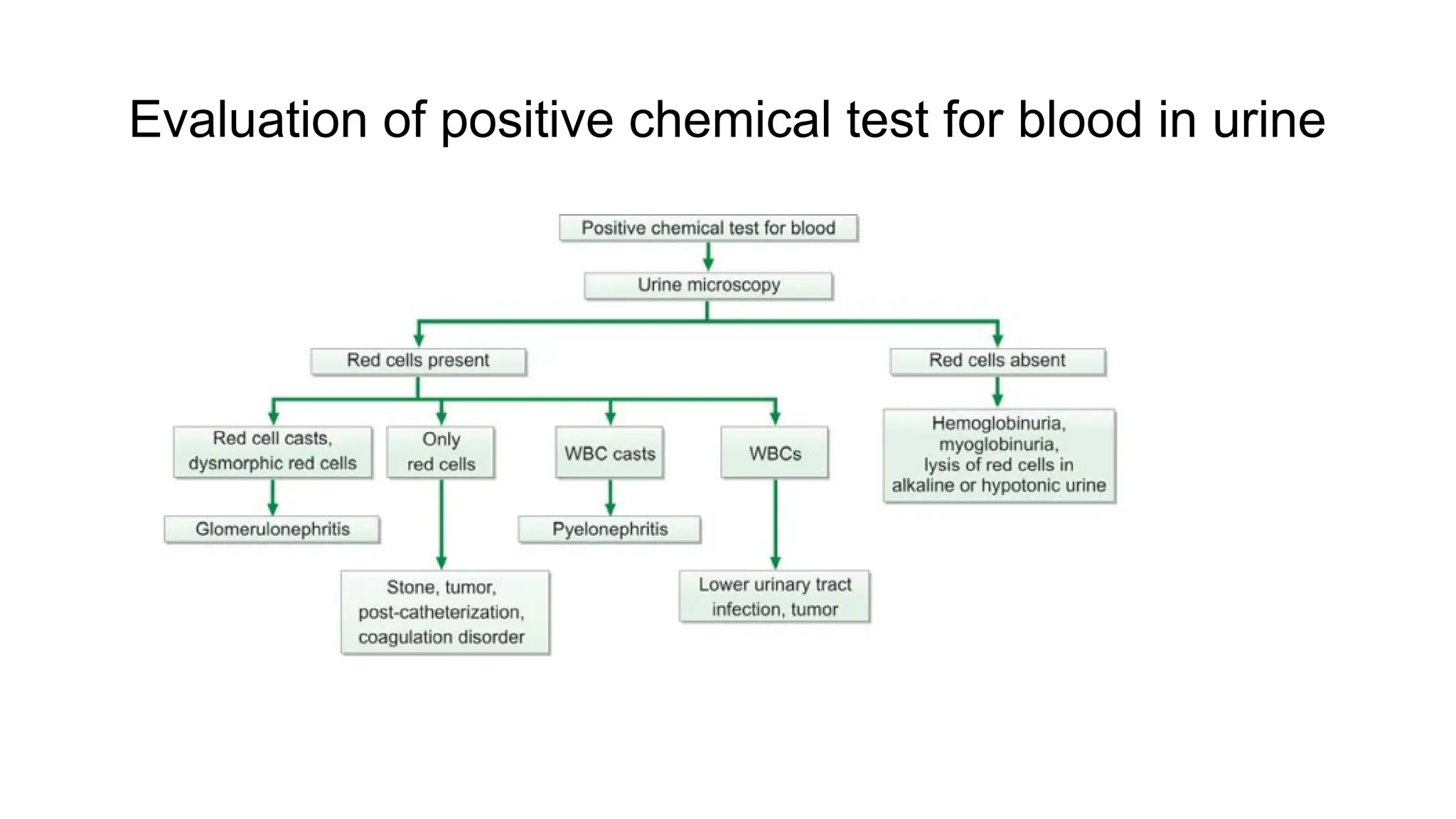
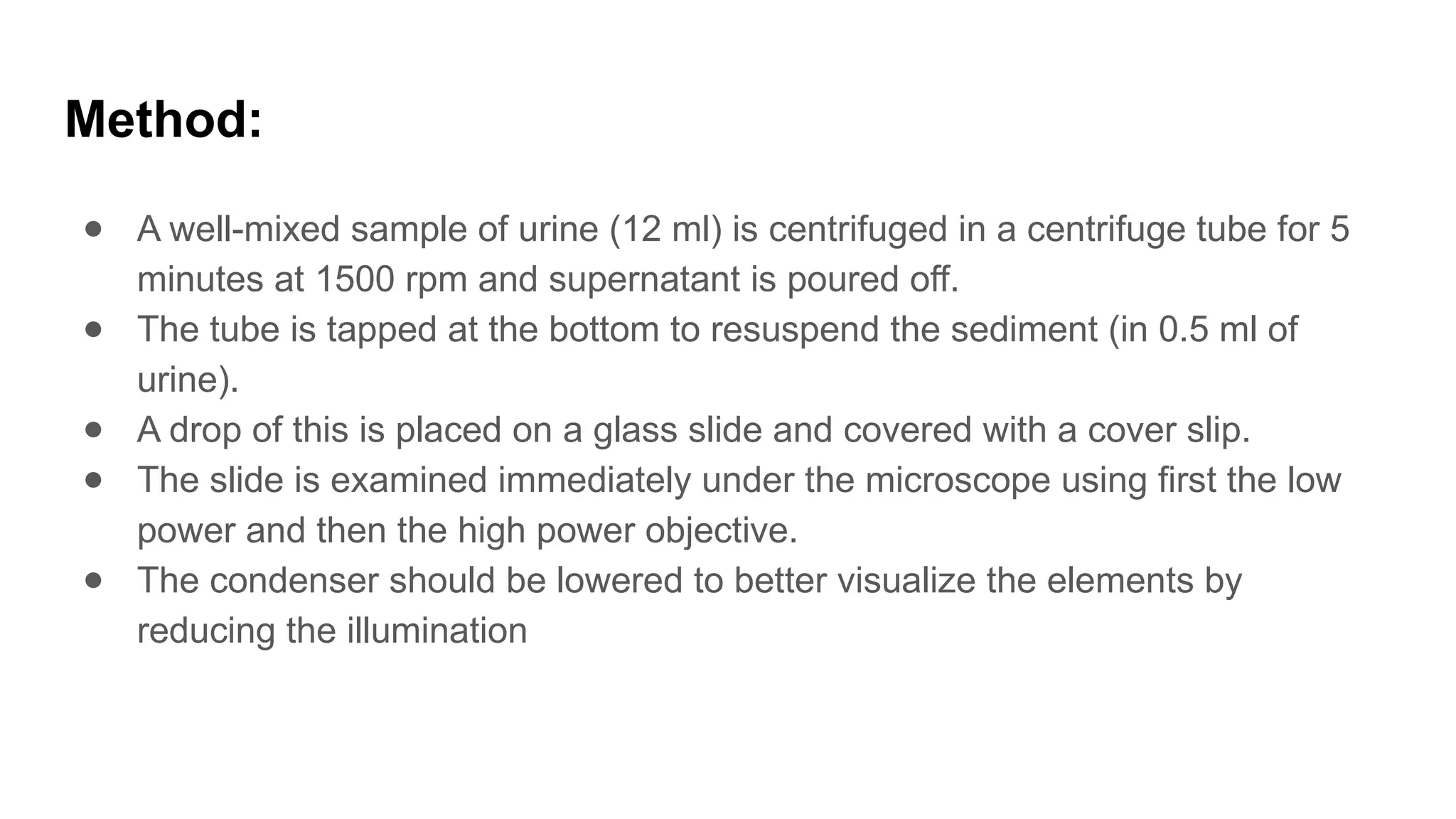
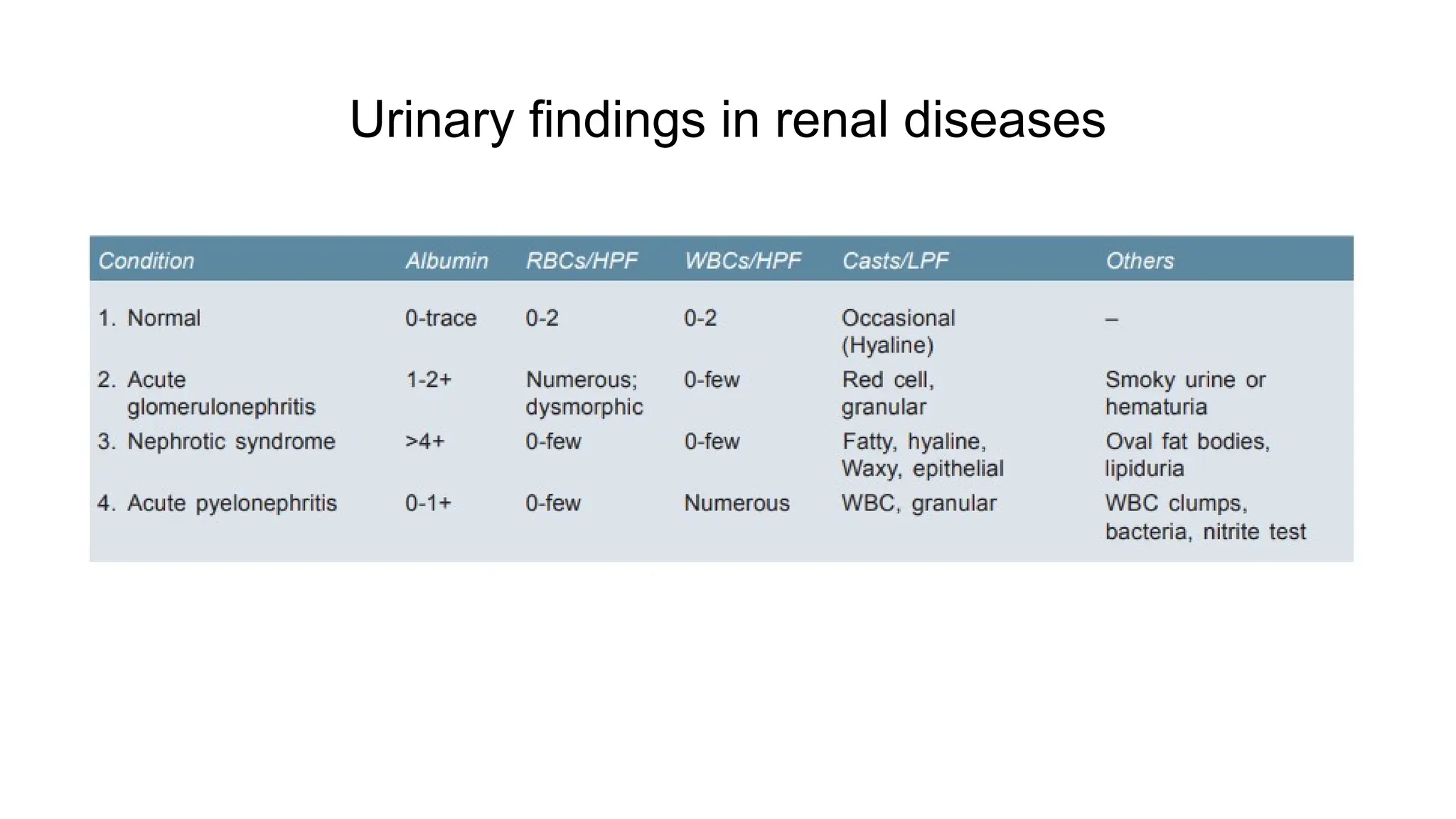
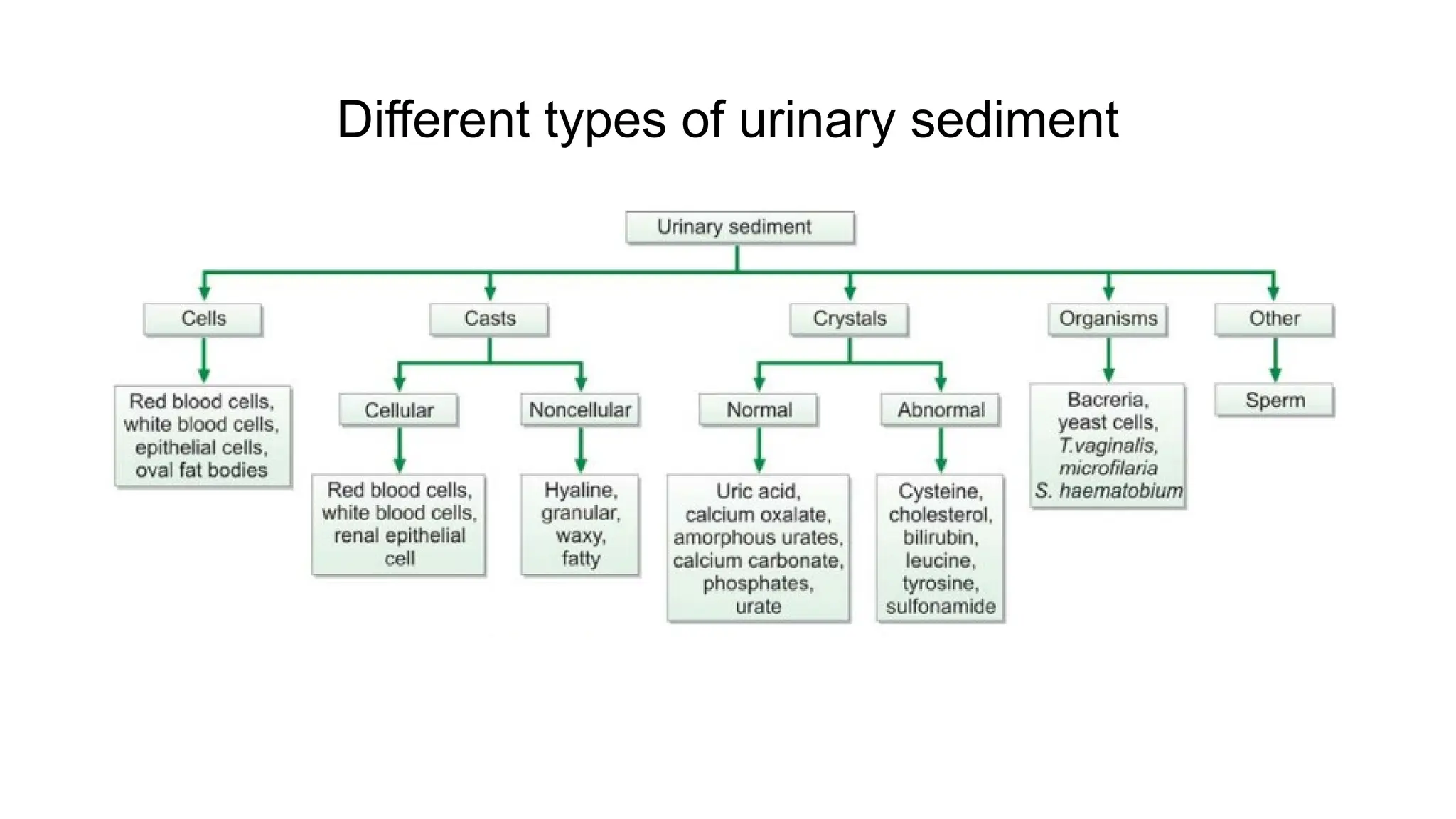
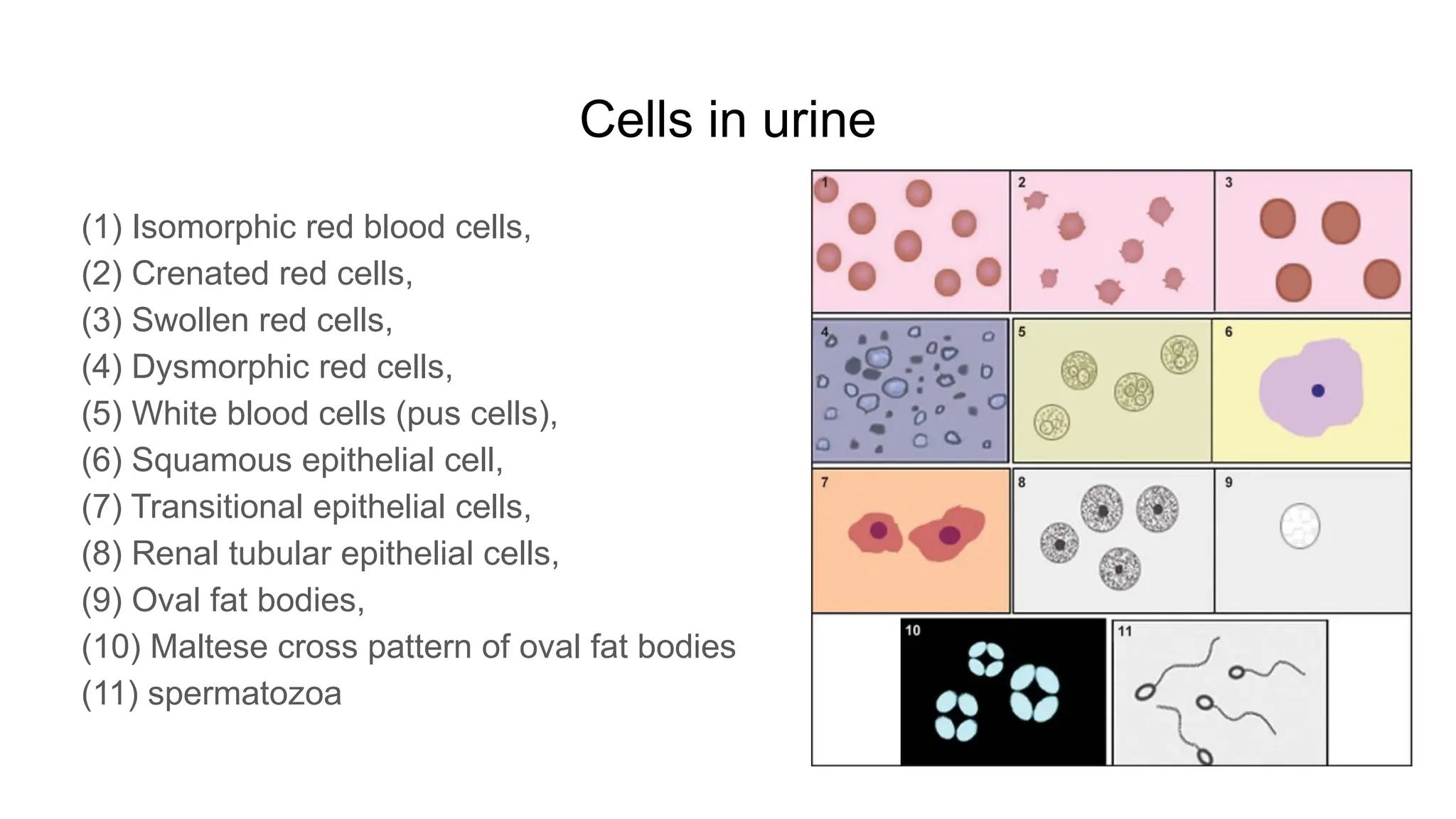
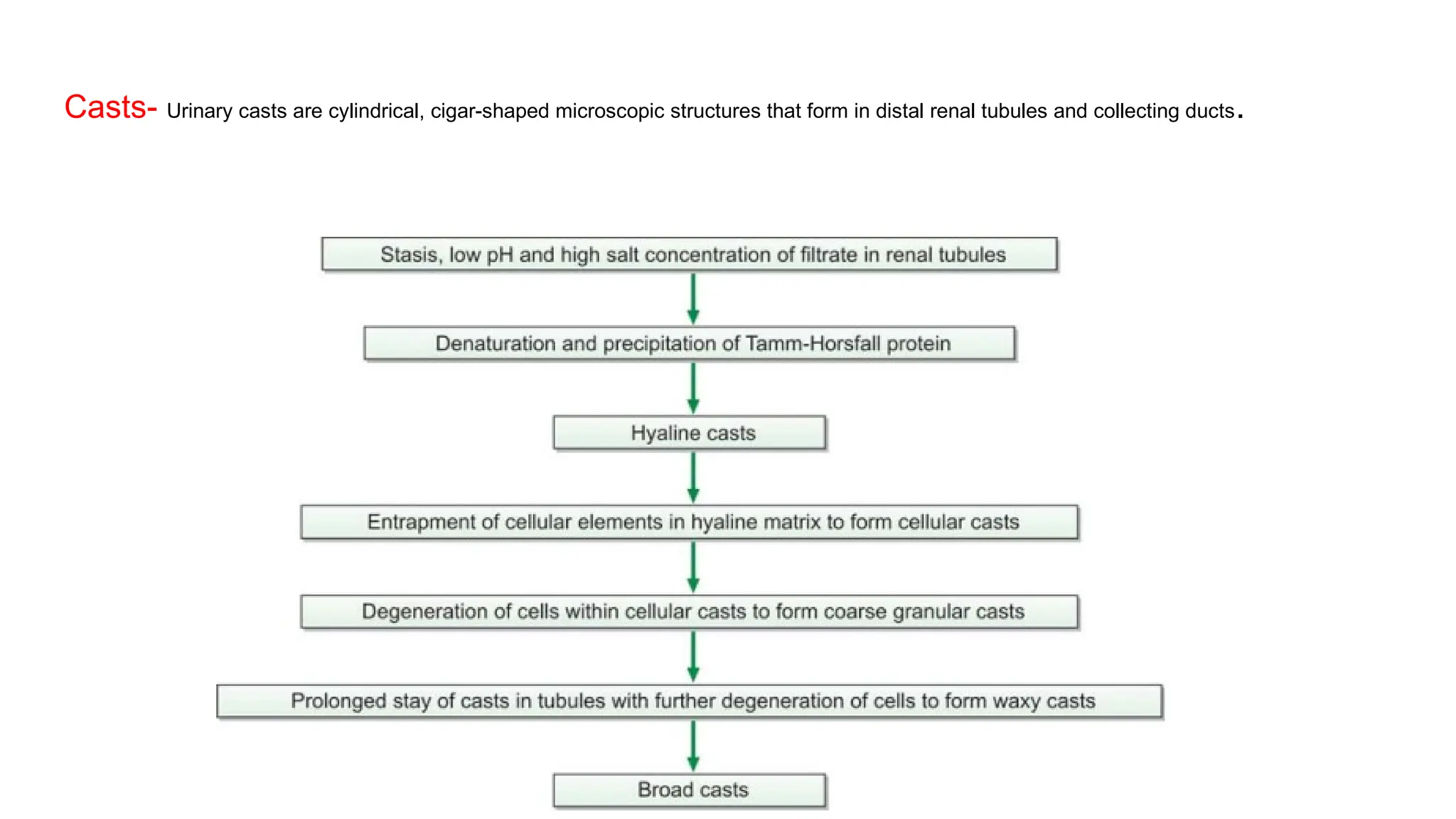
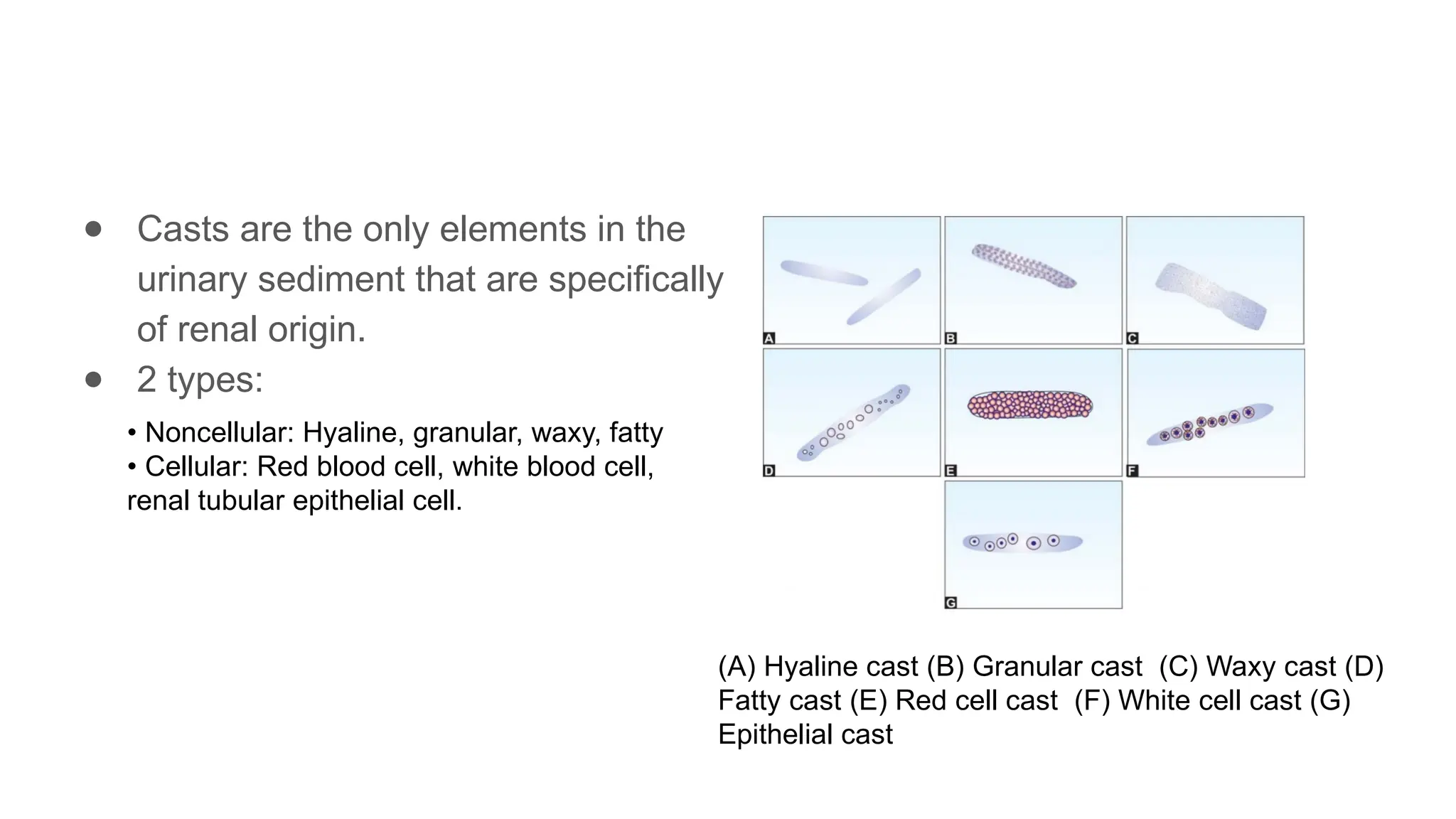
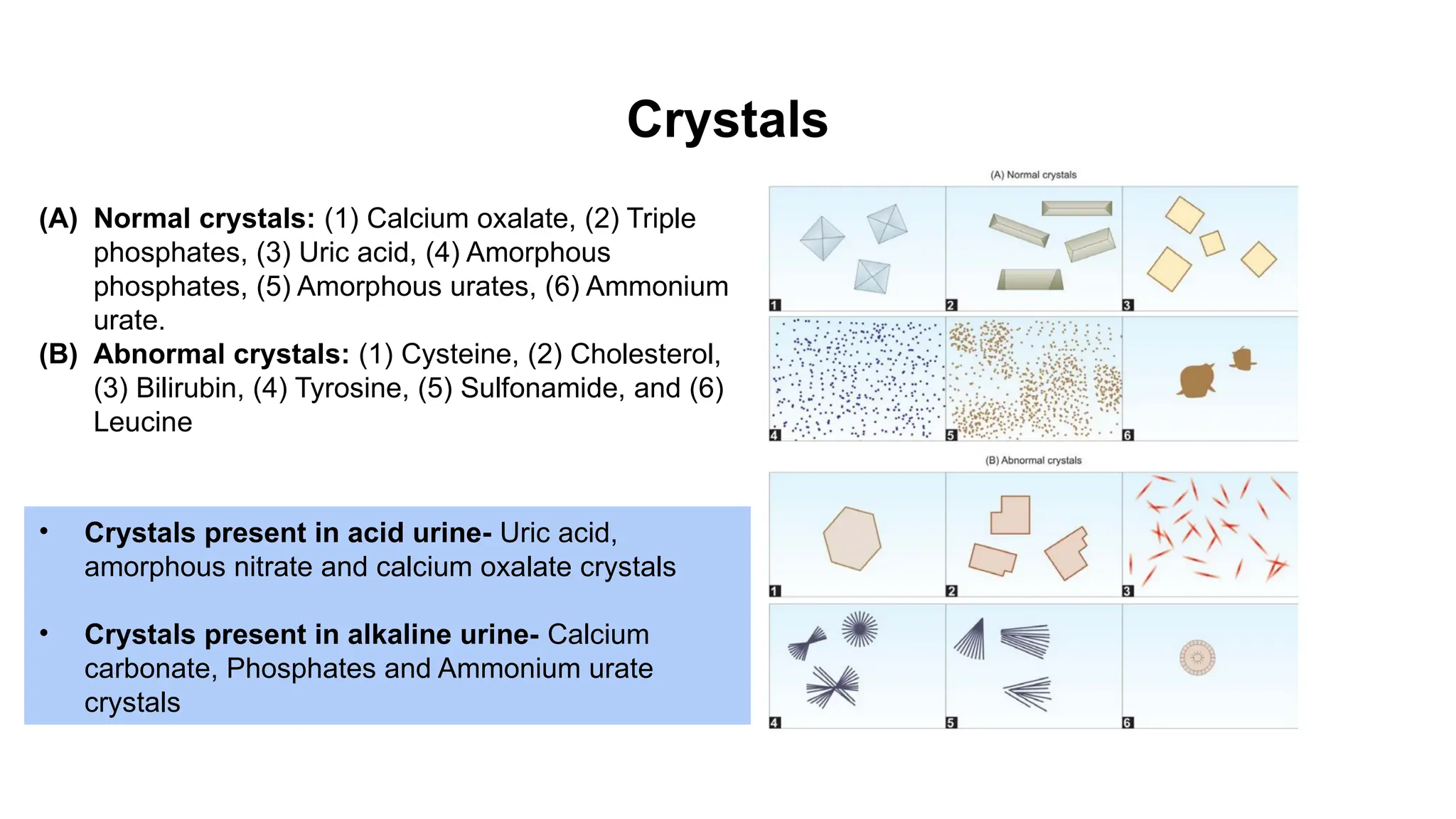
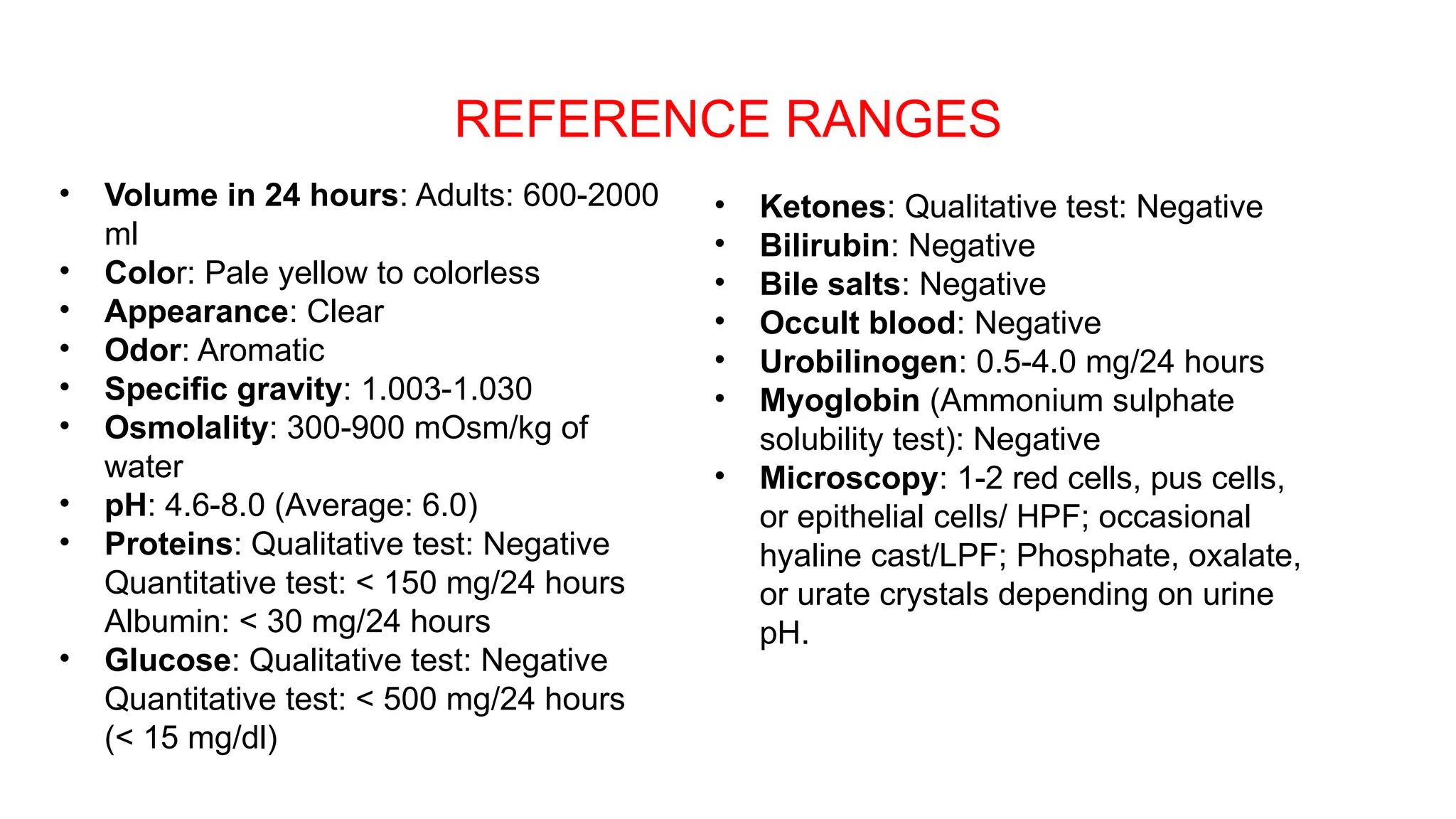
The document outlines the principles, collection methods, and interpretation of routine urine examinations. It details the various types of urine samples (e.g., first morning, midstream, 24-hour), normal values for urine characteristics (color, appearance, specific gravity, pH), and the significance of abnormal findings related to proteins, glucose, ketones, bilirubin, and blood. It also describes the methods for detecting these abnormalities and the implications of different findings in relation to various medical conditions.