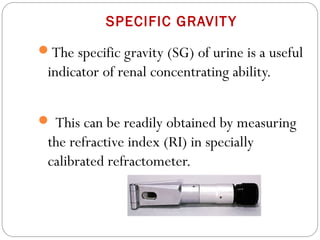
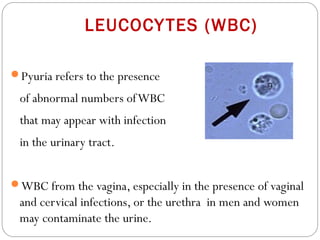
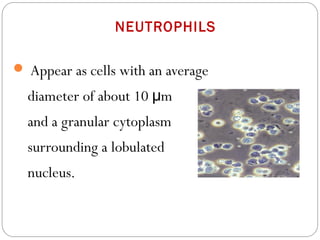
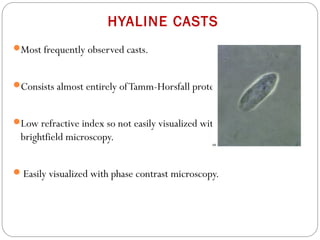
This document provides information on urine analysis and examination. It discusses the importance of analyzing urine promptly after collection and outlines appropriate collection, storage, and examination methods. Physical, biochemical, and microscopic tests are described in detail. Key findings are interpreted, such as the clinical significance of various cells, casts, crystals, and substances that may be present in urine. Proper collection and handling of urine specimens is also reviewed. The document aims to serve as a guide for physicians on evaluating urine as an important diagnostic tool.