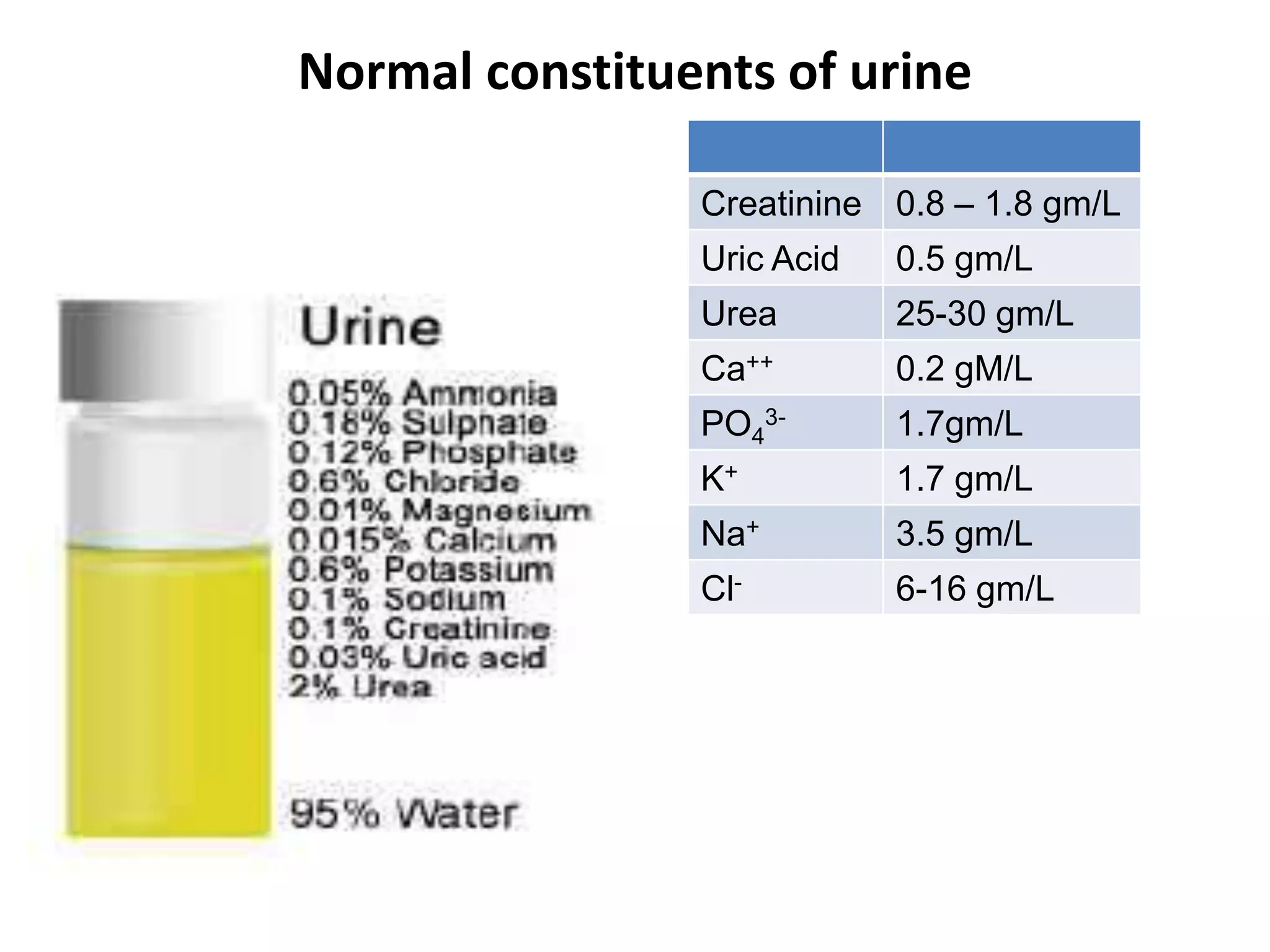
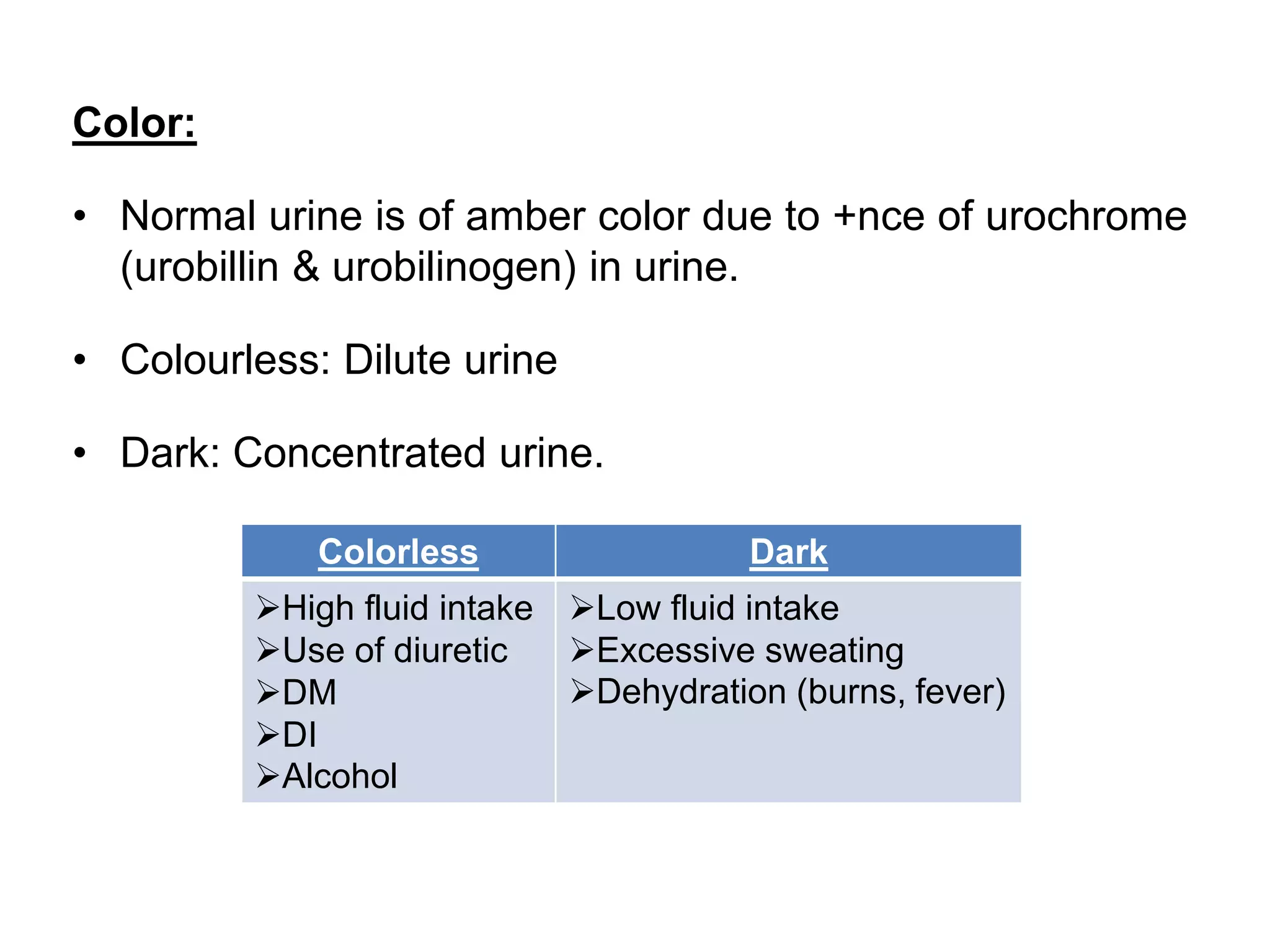
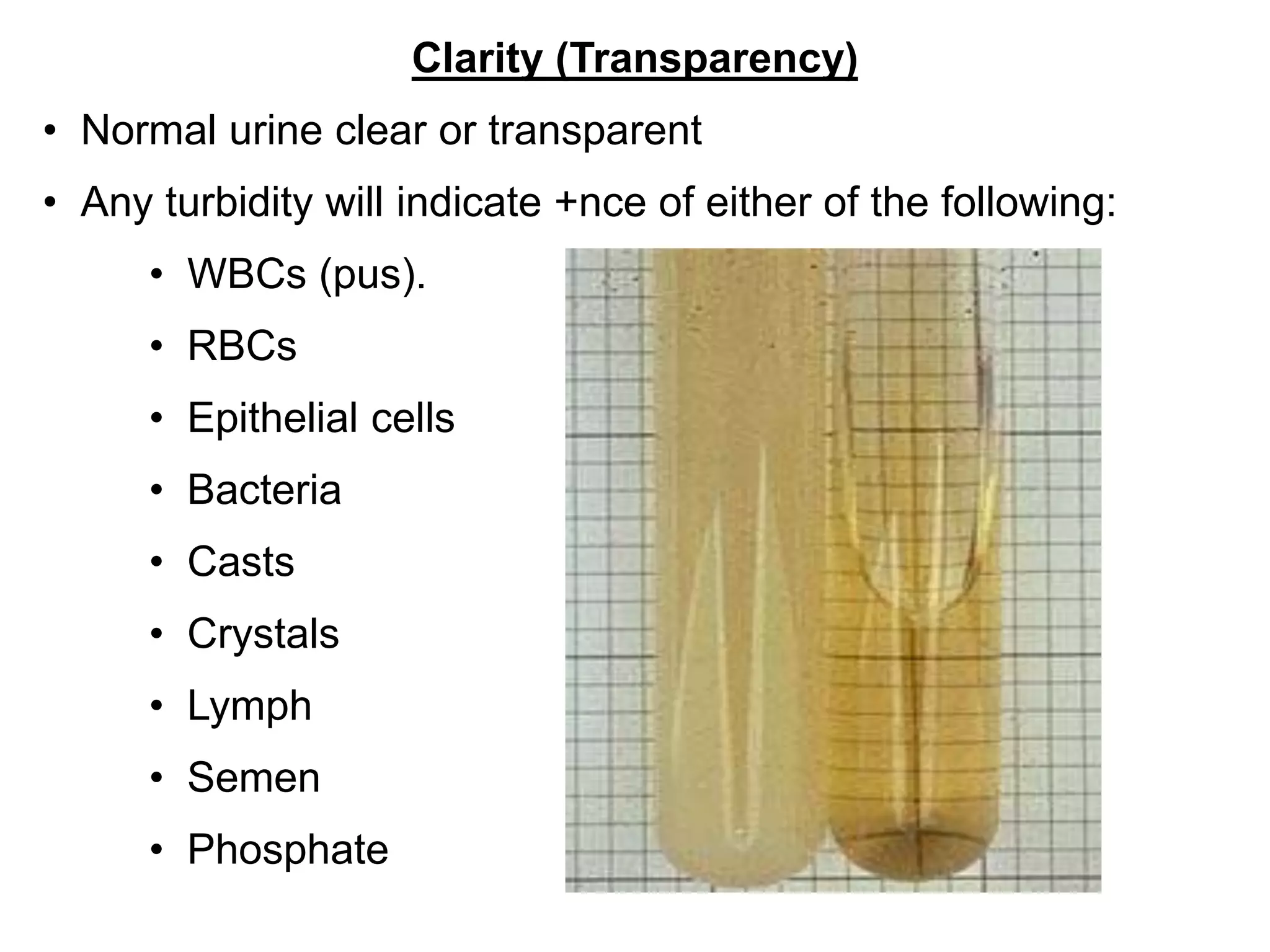
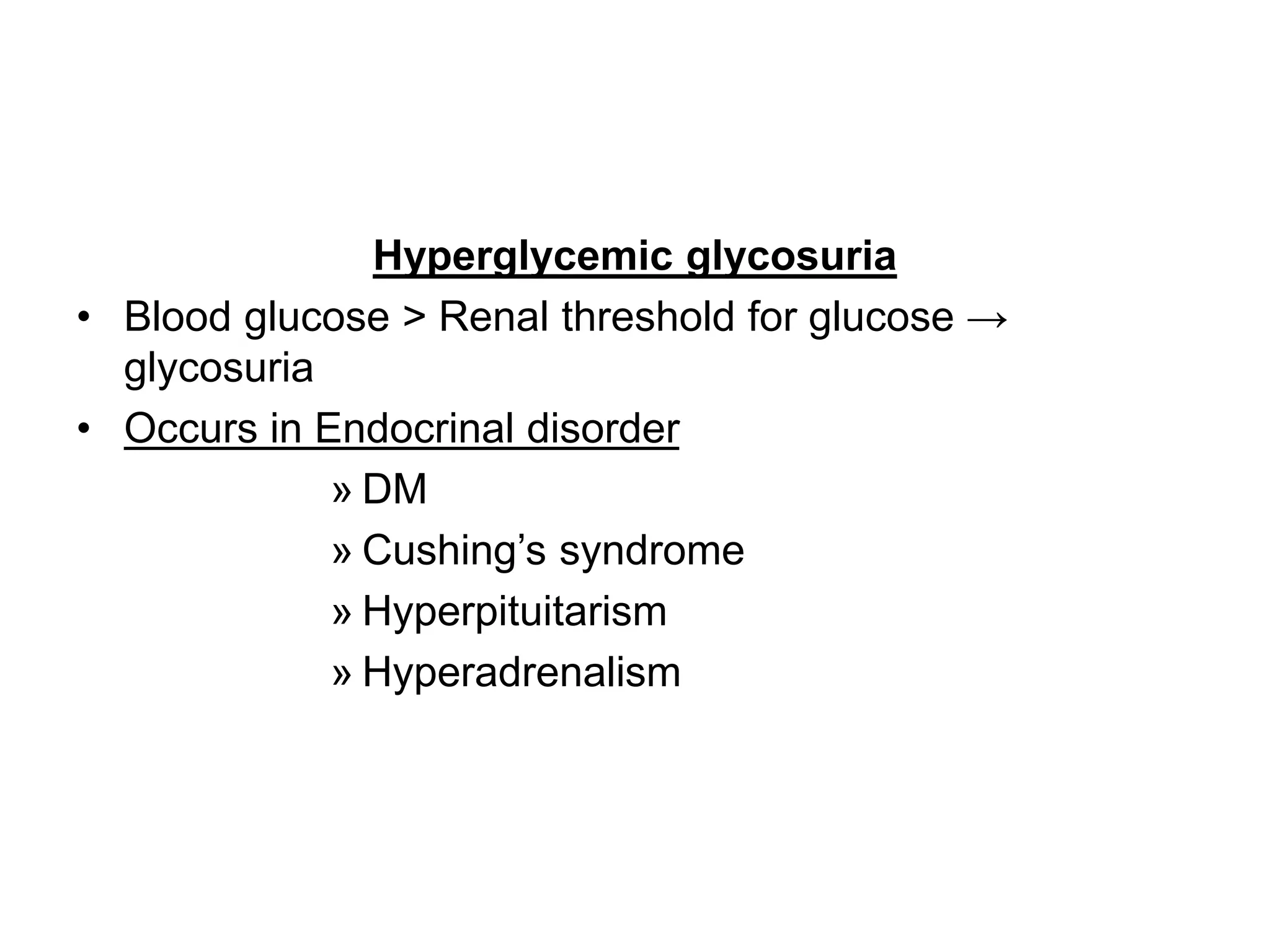
This document provides information on analyzing the constituents found in normal and abnormal human urine. It lists the normal ranges for creatinine, uric acid, urea, and other electrolytes found in urine. It also describes various tests used to detect abnormalities in urine like glucose, ketones, proteins, and bile constituents. Physical characteristics of urine like color, clarity, odor and their clinical significance are explained. Factors affecting the preservation of urine specimens and how they change if not preserved properly are also summarized.

![• Urine
– Water (95%) & Solids (5%)]
– Urinary out put: 1-1.5 L per day.
– Almost all substances found in urine are also find in
blood.
– may also contain cells, casts, crystals, mucus &
bacteria.](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-2-2048.jpg)
![• Urine:
– Provides information about functioning &
abnormalities of kidneys & urinary tract
– Help in diagnosis of various systemic diseases [+nce
or –nce of several substances in urine]](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-3-2048.jpg)

![• Chemicals used
– Toluene
– Thymol [for sugar estimation]
– Formalin
– Boric acid
– Camphor
– Toluol [for acetone estimation]
– Chloroform](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-6-2048.jpg)



![Abnormal colour of urine
11
Cloudy Excess PO4, Urates, Pus cells, Bacterial contamination
Red Frank Hematuria, hemoglobinuria, Myoglobinuria,
Intake of Pyridium, Phenolphthalein
Ingestion of Beet root, Black berries
Deep yellow Obstructive Jaundice, Ingestion of Vitamin B complex
Greenish Obst. Jaundice [excess Billirubin or billiverdin]
Phenol poisoning
Blue Methylene Blue poisoning
Brown black Hemorrhage in bleeding, Acidic urine, Porphyria
Black Alkaptonuria
Milky +nce of Chyle
Cola Nephritic syndrome](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-11-2048.jpg)

![VOLUME
Adult 600 – 2500 ml /24hr 0.5-1ml /kg/hr ~ 1.5L/24hr
Children 200–400ml/24hr 4ml/kg/ hr
Oligouria ↓ in urine flow [< 400 ml]
Polyuria ↑ in urine flow [> 2500 ml]
Anuria <100ml/day
Nocturia ↑ urination during night](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-14-2048.jpg)

![Causes of polyuria:
↑ed fluid intake
↑ed salt & protein intake
Addison’s disease
Intravenous saline or glucose
Chronic glomerulonephritis
Diuretics intake
Psychogenic polydipsia
DM
DI
Causes of Oliguria:
Water deprivation
Dehydration
Prolonged vomiting
Diarrohea
Excessive sweating
Acute renal failure
Hypotension
Renal Ischemia
Obstruction
[Calculi,Tumor, Prostatic hypertrophy]](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-16-2048.jpg)
![• pH
– One of imp. functions of kidney is pH regulation.
– Blood pH: 7.4 & urine pH: ~ 6.0 (4.6 – 8.0)
[due to secretion of H+ & reabsorption of HCO3
-]
– Urine pH ≥ 9, indicate that urine is stand for a long
time & must be rejected.
Acidic urine Alkaline urine
Acidosis Alkalosis
DKA UTI [Proteus]
Starvation RTA
Dehydration Vegetarian diet
Diarrhea
E. coli infection
Muscular fatigue](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-17-2048.jpg)

![Specific gravity
• Normal: 1.015-1.025.
• Theoretical extremes: 1.003 to 1.032.
• Contamination during collection & storage gives false value.
Sp. gravity is ↓ed in
•Excessive water intake
•DI
•Chronic glomerulonephritis
•All cases of polyuria [except DM]
Sp. gravity is ↑ed in
•DM [Glycosuria]
•Nephrosis [Albuminuria]
•All cases of oliguria
•Hematuria
•Hemoglobinuria
•Execessive sweating](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-19-2048.jpg)


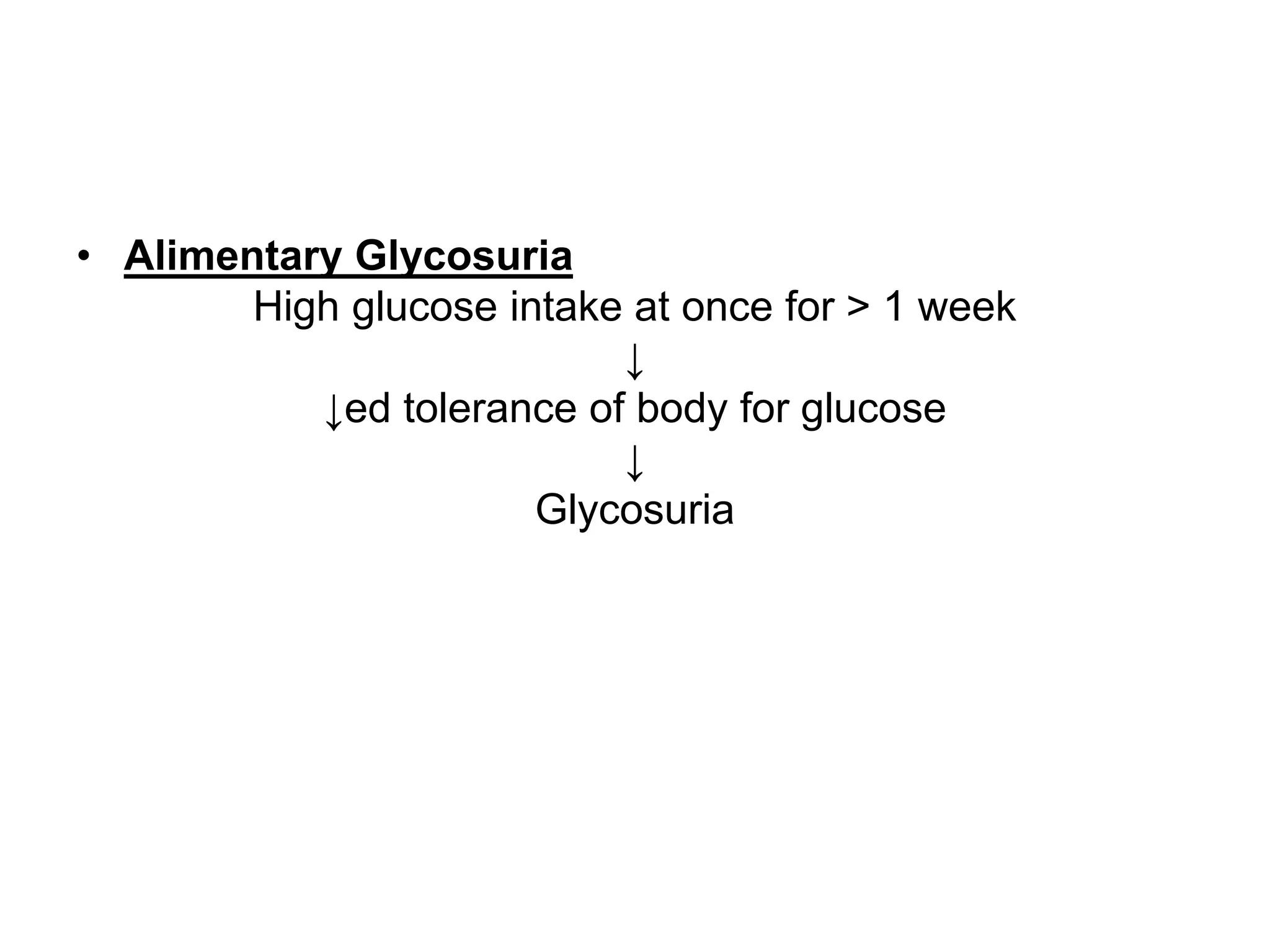
![• Urine examination for +nce of Sugar
– Glycosuria is defined as presence of sugar in urine in
a amount that can be detected by chemical methods.
– Reducing subst. found in urine:
Sugar Non-sugar
Glucose [DM, Endocrine disorder] CHCl3, Formaldehyde [preservative]
Lactose [Pregnancy, Lactation] Homogentistic acid
Fructose Ascorbic acid](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-22-2048.jpg)

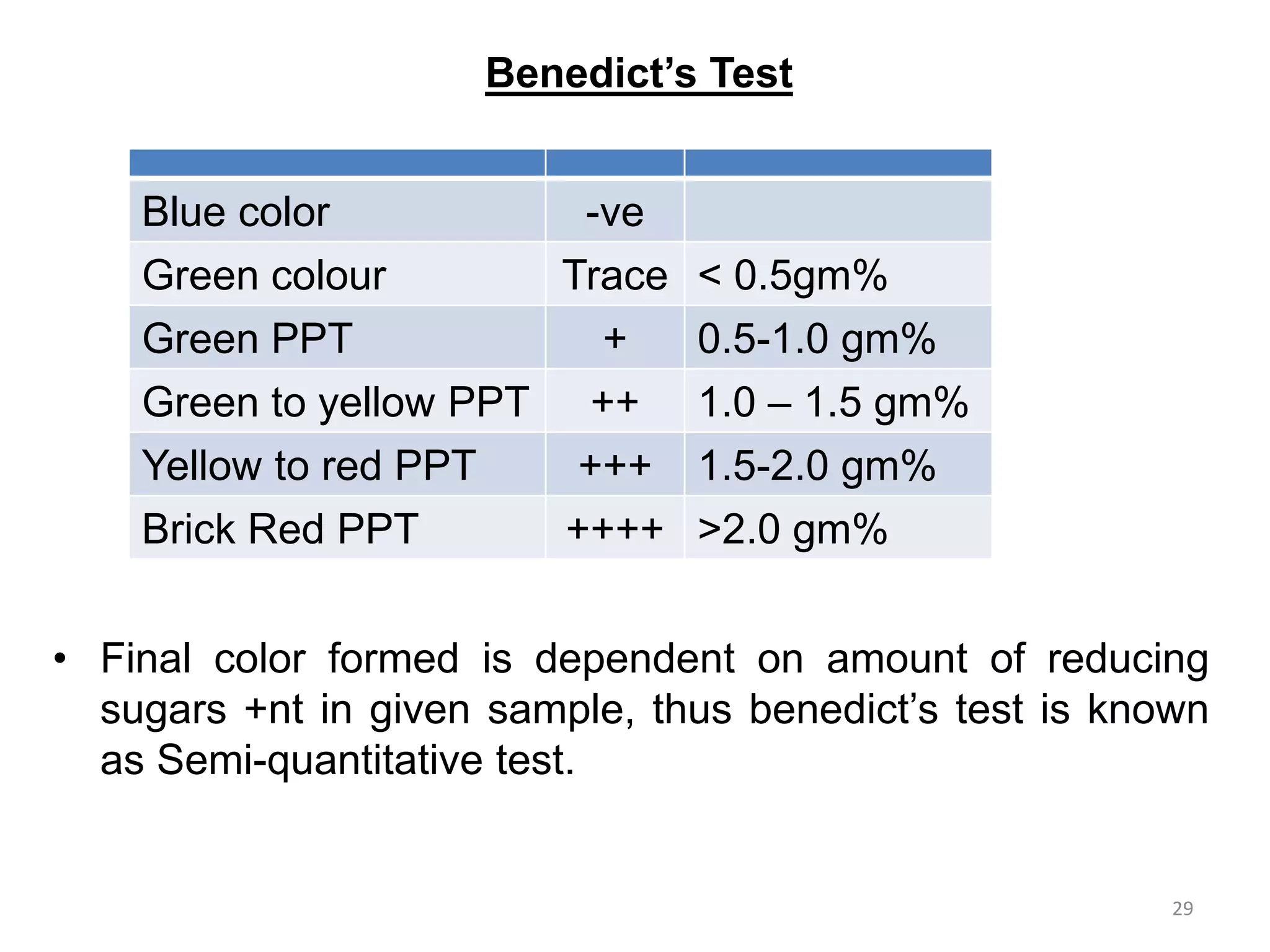
![Benedict’s Test
• General test for Reducing sugars
• Reagent’s composition:
26
CuSO4 17.3gm Provide Cu++
Na2CO3 100gm Provide alkaline medium
Na-Citrate 173gm Cu++ chelating agent [slowly releases Cu++ ]
Dist. water 1000ml](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-26-2048.jpg)


![KETONURIA
• Usually found ketone bodies in human body & urine are:-
β-Hydroxy butyrate --Acetoacetate------ Acetone
[Primary]
• Normal level of ketone bodies in blood: 70mg/dl
• Renal threshold for ketone bodies: 1mg/dl
• normallly excreted in urine. [<20mg/day]
↑ed KB in urine
Intake of high fat & low carbohydrate diet
Starvation
Uncontrolled DM
Prolonged vomiting](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-30-2048.jpg)
![• Rothera’s test [Nitroprusside test]
– Reagents:
(NH4)2SO4 Crystals Precipitate protein
NH3 solution Provide alkaline medium
Freshly prepared 5% Na-Nitroprusside solution](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-31-2048.jpg)
![• Rothera’s test [Nitroprusside test]
– Principle: Saturation of urine with (NH4)2SO4 leads
to settling down of proteins as precipitate.
– KB remains at surface.
– In alkaline medium, KB reacts with sodium
Nitroprusside to give purple/pink ring (at interface).](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-32-2048.jpg)
![• Rothera’s test [Nitroprusside test]
– Procedure:
– 2 mL of urine was taken in a test tube.
– 3 drops of nitroprusside solution was added to it.
– 2 mL of NH3 solution was added slowly along the
side wall of tube.
Observation Inference
Sample A
Sample B](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-33-2048.jpg)
![Urinary protein (proteinuria)
• Tamm horse fall protein: protein normally found in urine
(<30 mg/24hr). [undetectable by routine methods]
• Proteinuria: defined as +nce of protein in urine that can be
detected by routine methods.
Pre renal Renal Post renal
Cardiac disease Glomerulonephritis Severe UTI
Fever Nephrotic syndrome Lesions of renal pelvis
Cancer Nephritic syndrome Lesions of bladder
Collagen disease Carcinoma of kidney Lesions of prostate
Intra-abdominal tomors Pyelonephritis Lesions of urethra
Rejection of kidney allograft](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-34-2048.jpg)

![• Glomerular
– Causes:
a. Immune complex deposition
b. AGE deposition [Diabetic Nephropathy]
– ↑ in glomerular permeability due to: ↑ in pore size of
glomerular memb. & loss of -ve charges due to podocyte foot
process retraction & basement memb. damage.
– >3.5gm/24hr: hallmark for diagnosis of Nephrotic
syndrome](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-36-2048.jpg)
![• Tubular
– Low mol. Wt. Proteins are normally filtered by
glomerulus & completely reabsorbed in PCT.
[eg: β2-microglobulin, Ig- light chains, & RBP]
Loss of tubular function
↓
↓ reabsorption
↓
Tubular proteinuria
– Causes: Toxic agents [Heavy metal, Drugs]](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-37-2048.jpg)






![• Bile pigments found in urine
In Normal urine [< 0.02mg%] In abnormal urine
•Urochrome [Chemical nature unknown]
•Traces of urobilin [Small amount can’t
be detected]
•Bilirubin [in freshly voided urine]
•Urobilinogen
•Biliverdin [develops on standing urine
from oxidation of bilirubin]
•Urobilin [decomposition product of
bilirubin or urobilinogen due to action of
light or action of bacteria]
• Significance of bilirubinuria
– Only conjugated bilirubin appears in urine.
– It occurs with even minimal degree of jaundice &
may be detected before clinical jaundice is evident.](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-44-2048.jpg)
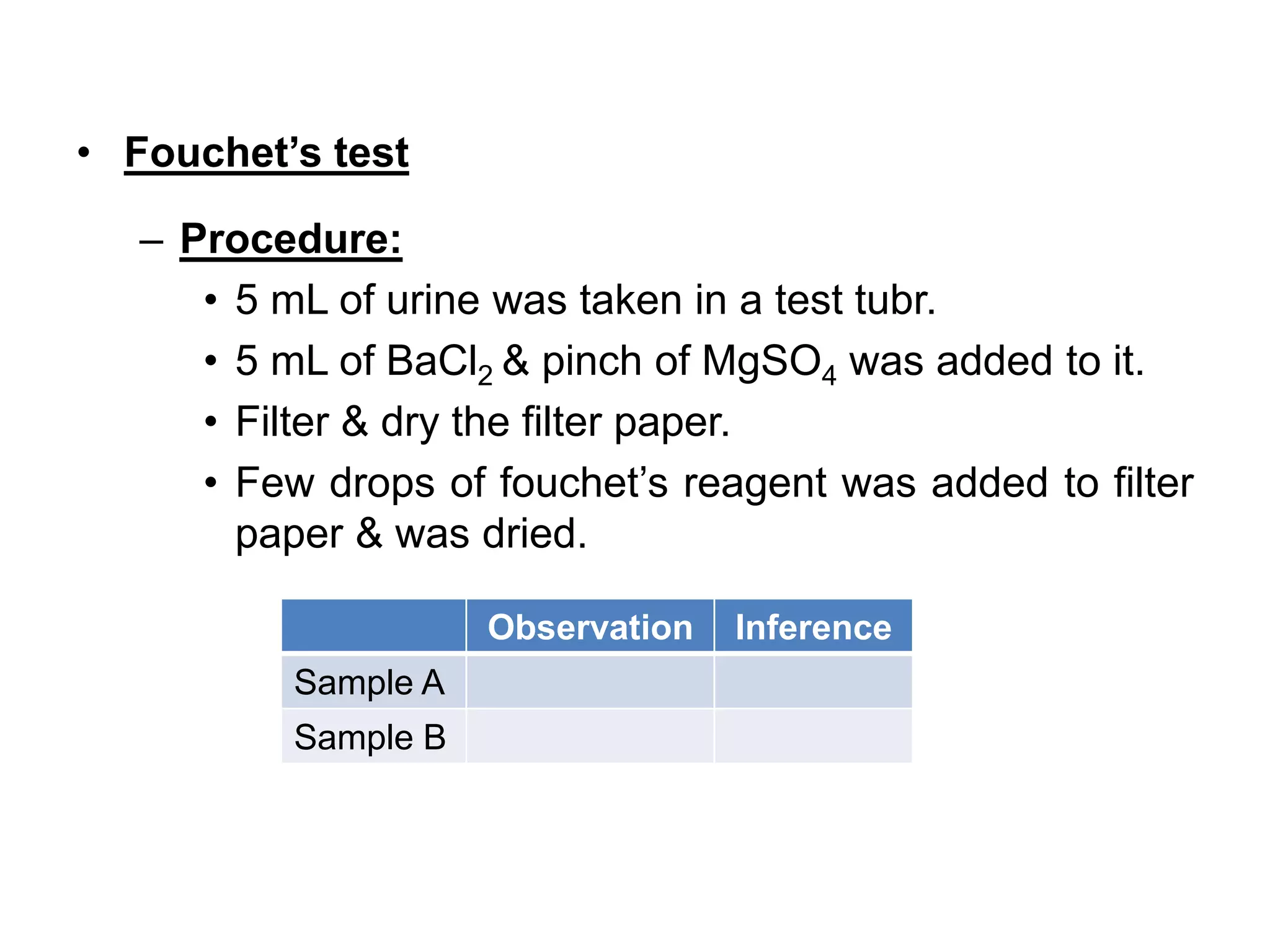
![• Fouchet’s test
– Reagents:
• 10% BaCl2
• Fouchet’s reagent [FeCl3 in TCA]
– Principle:
• BaCl2 react with sulphate radicals in urine to form
BaSO4.
• Bile pigment gets adhered toBaSO4.
• Bilirubin (yellow) is oxidised to biliverdin (green)
with FeCl3 in presence of TCA.](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-45-2048.jpg)

![Hay’s surface tension test [Sulphor test]
• Reagent:
– Sulphor powder
• Principle:
– Presence of bile salts ↓es surface tension of urine
allowing sulphor powder to sink.
False +ve hay’s test False -ve hay’s test
CHCl3 Thymol
Turpentine Excess urobilin in urine](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-48-2048.jpg)
![Hay’s surface tension test [Sulphor test]
• Procedure:
– 4mL of urine was taken in a test tube.
– A pinch of sulphor powder was sprinkled on the
surface of urine.
Observation Inference
Sample A
Sample B](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-49-2048.jpg)





![• Hemoglobinuria
Blood Hb > Hb binding capacity of haptoglobin
↓
Hb filtered
↓
Hb appears in urine
[Hemoglobinuria]
– Occurs in:
Malaria
Septicemia [hemolytic streptococcal infection]
Sickle cell anemia
Thallasemia
Incompatible blood transfusion
Effect of chemicals on RBC [Sulphonamide, Phenylhydrazine, Arsenic, etc]](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-55-2048.jpg)
![• Myoglobinuria
Injury to cardiac/ skeletal muscle
↓
Mb released
↓
Excreted via urine
• Mb: toxic to kidney [high concentration may lead to Acute
renal failure.
MI
Infarction of large skeletal muscle
Muscle damage [Injury, Electric shock, Heat stroke]
Trauma](https://image.slidesharecdn.com/urinepractical-200121115146/75/Abnormal-Constituents-of-Urine-practical-56-2048.jpg)