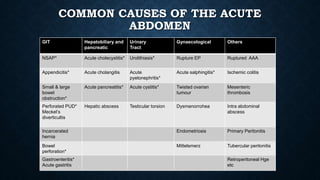
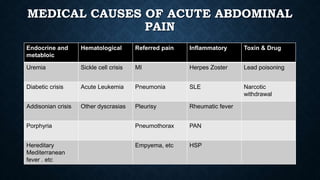
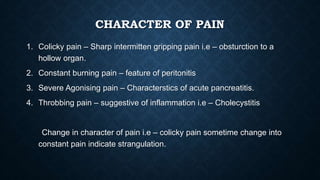
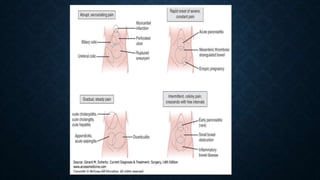
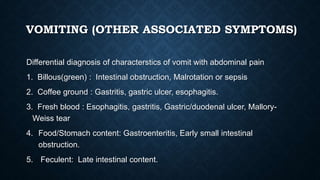
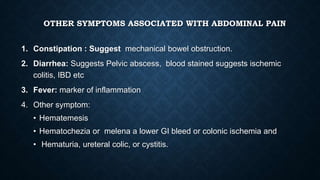
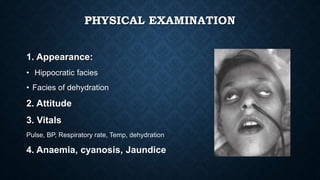
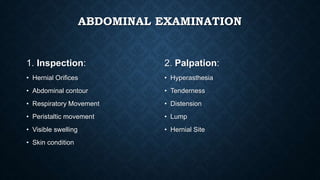
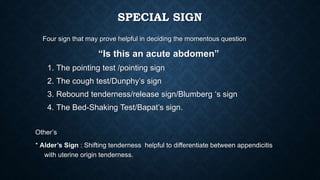
This document discusses the diagnosis and management of acute abdominal pain. It defines acute abdomen as sudden abdominal pain lasting less than 24 hours. Common causes are appendicitis, cholecystitis, intestinal obstruction, and perforated viscus. A thorough history, physical exam, and lab/imaging workup is needed to diagnose the specific cause as treatment depends on the etiology. Laparoscopy can help diagnose unclear cases or distinguish surgical from non-surgical conditions. The goal is to determine if the patient requires immediate surgery, surgical observation, medical management, or further diagnostics.