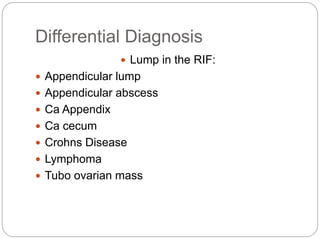
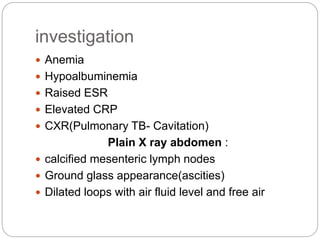
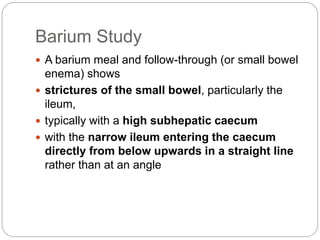
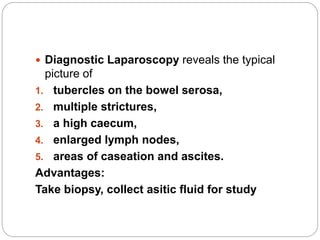
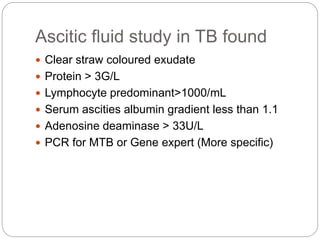
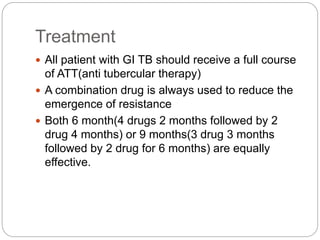
This document discusses abdominal tuberculosis (TB), which involves the GI tract, peritoneum, lymph nodes, or solid organs like the liver and spleen. It describes the types of intestinal TB (primary vs secondary), presentations, investigations, and treatments. Primary intestinal TB develops in an unexposed person from infected milk, while secondary TB arises from reactivation of dormant lesions. Symptoms include fever, weight loss, abdominal pain, diarrhea, and distension. Diagnosis involves lab tests showing anemia and inflammation as well as imaging studies. Treatment is a full course of anti-TB drugs, with surgery only for complications like obstruction or perforation.