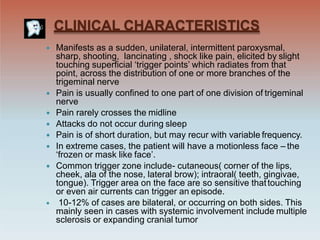
Neuralgia is severe pain along the path of a nerve that is usually caused by damage to the nerve. Trigeminal neuralgia, also called tic douloureux, is a specific type of neuralgia that causes severe facial pain. It is characterized by sudden, severe, sharp pain in the face that is triggered by everyday activities like talking, eating, or brushing teeth. Trigeminal neuralgia is often caused by compression of trigeminal nerve roots from blood vessels, and treatments include medications like carbamazepine or surgery to decompress the nerve. Differential diagnosis considers other conditions like dental pain, sinusitis, or tumors that can mimic trigeminal neuralgia symptoms.