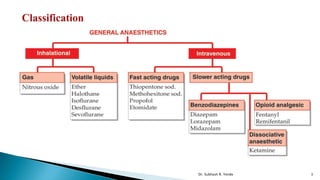
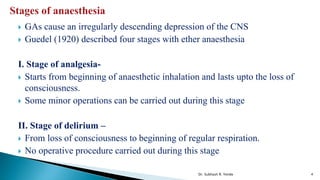
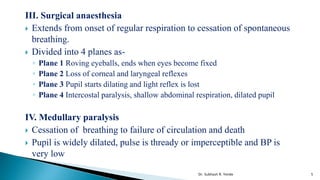
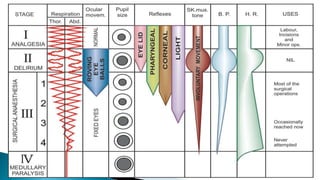
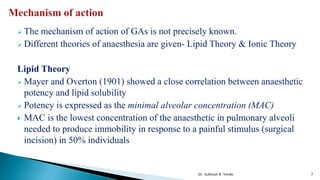
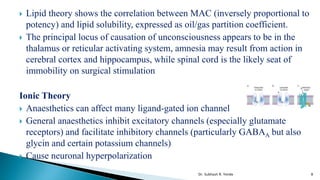
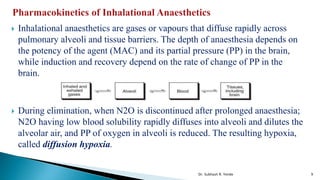
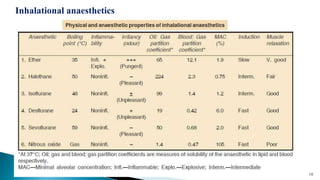
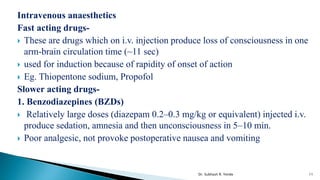
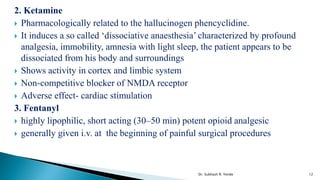
The document discusses general anesthetics and their mechanisms of action. It describes the four stages of anesthesia identified by Guedel using ether as an example. The two main theories for how general anesthetics work are the lipid theory and ionic theory. It also discusses inhalational and intravenous anesthetics, including examples like thiopentone sodium, propofol, benzodiazepines, ketamine and fentanyl. Finally, it covers preanesthetic medication and examples of drugs commonly used.