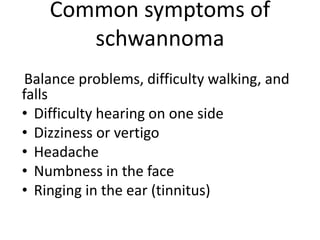
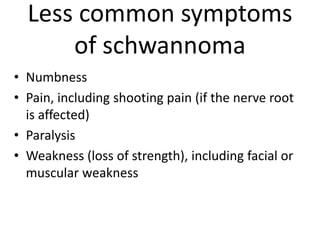
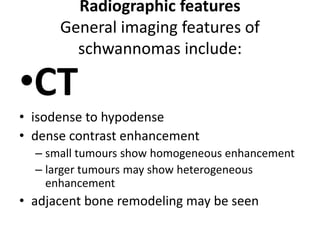
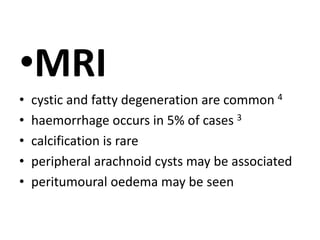
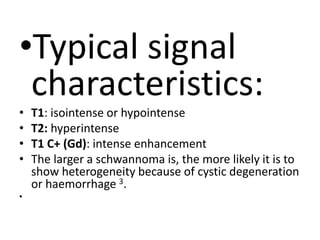
Schwannoma is a benign tumor that develops from Schwann cells covering nerves. It most commonly involves cranial nerves VIII (acoustic neuroma) and V. Symptoms depend on the affected nerve but may include hearing loss, dizziness, facial numbness, and headaches. Schwannomas typically appear iso- to hypointense on T1-weighted MRI and hyperintense on T2-weighted MRI, demonstrating intense contrast enhancement. Surgery is the primary treatment and prognosis is generally good, with low recurrence risk even after complete resection.