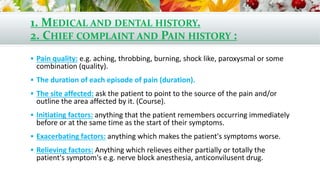
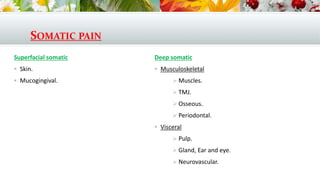
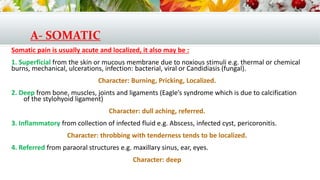
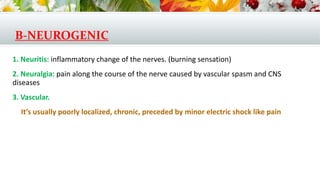
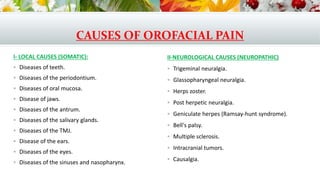
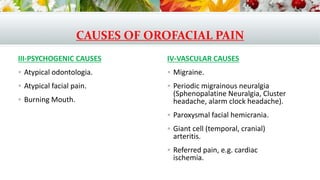
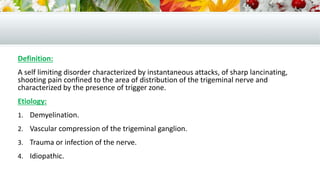
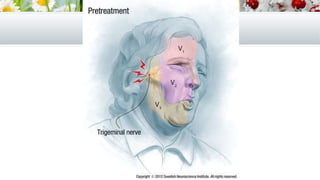
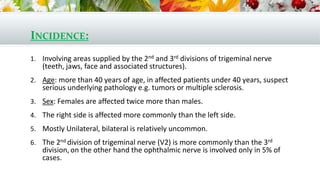
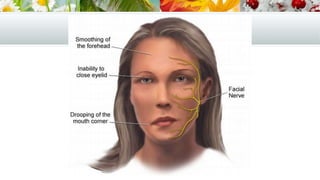
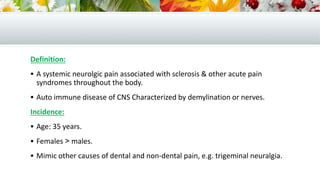
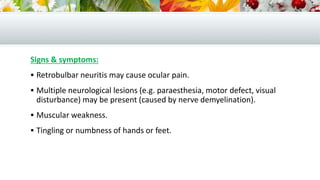
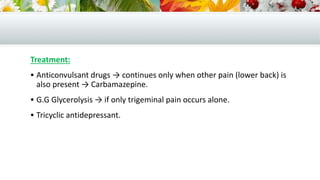
1. The document discusses various types of orofacial pain including somatic, neurogenic, and psychogenic pain. It describes trigeminal neuralgia as a common type of neurogenic pain characterized by sharp, electric shock-like pain in the face that is triggered by stimulation of specific trigger zones. 2. Evaluation of orofacial pain involves taking a thorough medical history and performing physical and neurological examinations. Differential diagnosis considers local causes as well as neurological disorders. 3. Treatment depends on the underlying cause but may include medications, nerve blocks, surgery, or a combination. Carbamazepine is first-line treatment for trigeminal neuralgia.