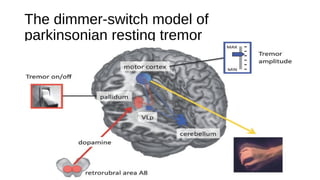
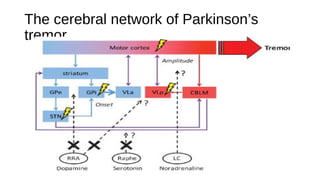
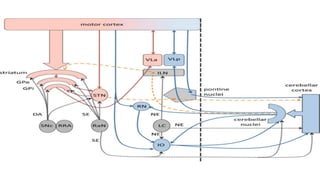
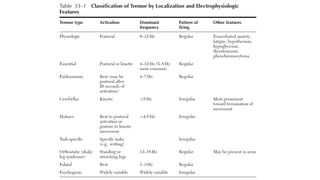
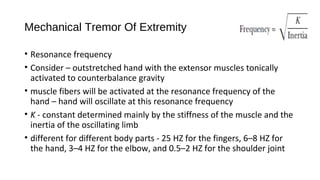
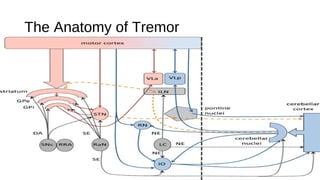
This document discusses the pathophysiology of tremor. It describes tremor as a rhythmic oscillation of a body part that can be characterized by the parts affected, frequency, and amplitude. There are four principles of tremor genesis: mechanical oscillation, reflex activation, central oscillators, and unstable feedforward/feedback loops. Resting tremor in Parkinson's disease involves dysfunction of the basal ganglia and cerebellar circuits. Action tremor has been linked to neurodegeneration in the cerebellum and changes in GABA signaling. Different types of tremors can result from lesions in specific areas like the cerebellum, midbrain, or brainstem.










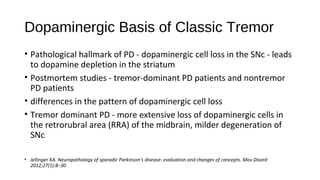

![• Nuclear imaging studies - [123I]FP-CIT SPECT
• Dopamine transporter (DAT) density in the striatum - correlates with
the severity of all motor symptoms, except resting tremor
• DAT density in the pallidum - correlated with tremor severity, but not
with bradykinesia or rigidity
• Hypothesized - specific loss of dopaminergic cells in the RRA -
produce pallidal dopamine depletion - resting tremor
• Helmich RC, Janssen MJR, Oyen WJG, Bloem BR, Toni I. Pallidal dysfunction drives a cerebellothalamic circuit into Parkinson
tremor. Ann Neurol 2011;69(2):269–281](https://image.slidesharecdn.com/g94qslmxtea2e5hoi8la-signature-d0060fa190e8ce3c0ef23e13247a289b690b683b6b9dfca6c7b486ed09835dac-poli-180408183006/85/Tremor-Pathophysiology-20-320.jpg)