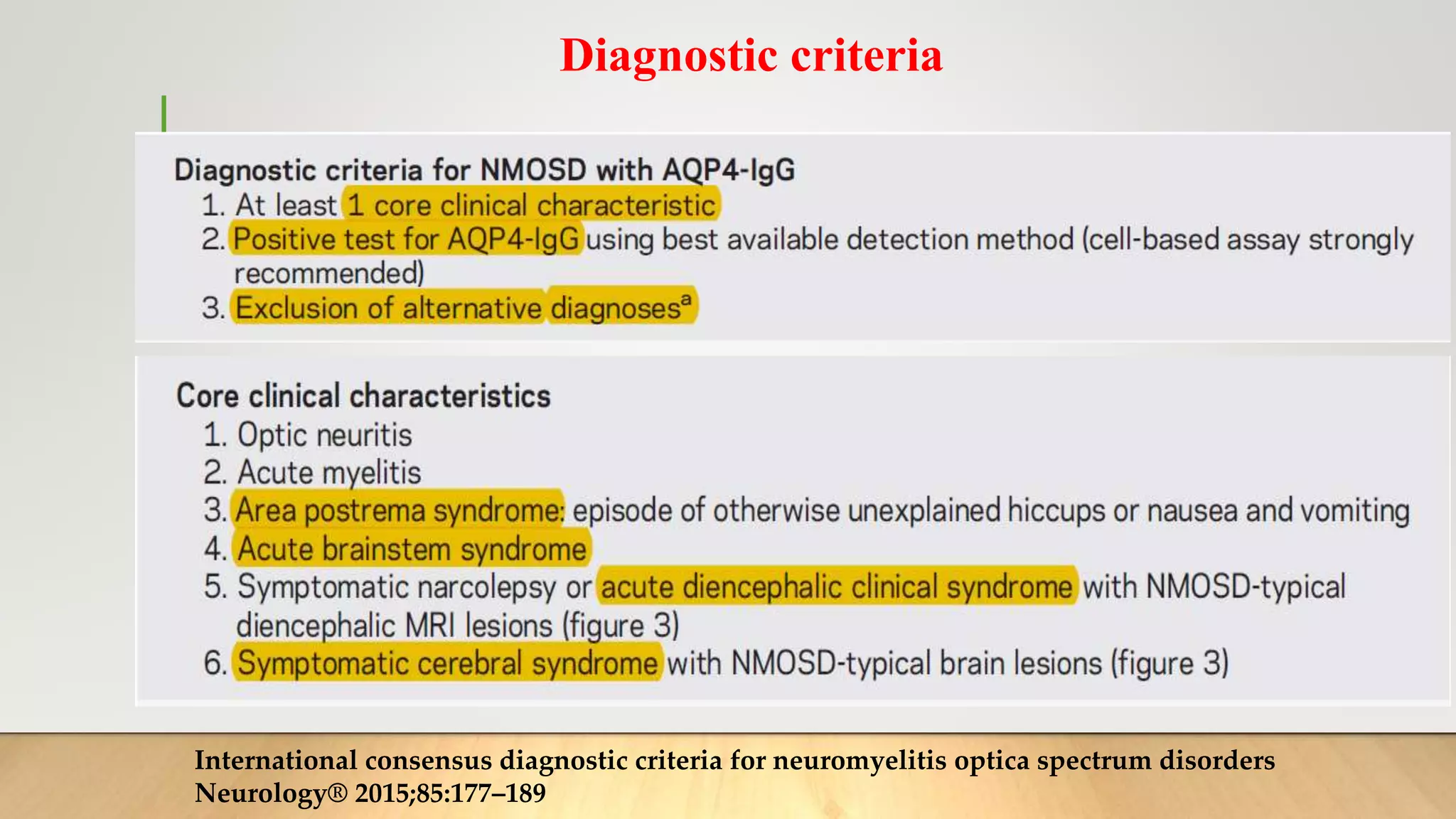
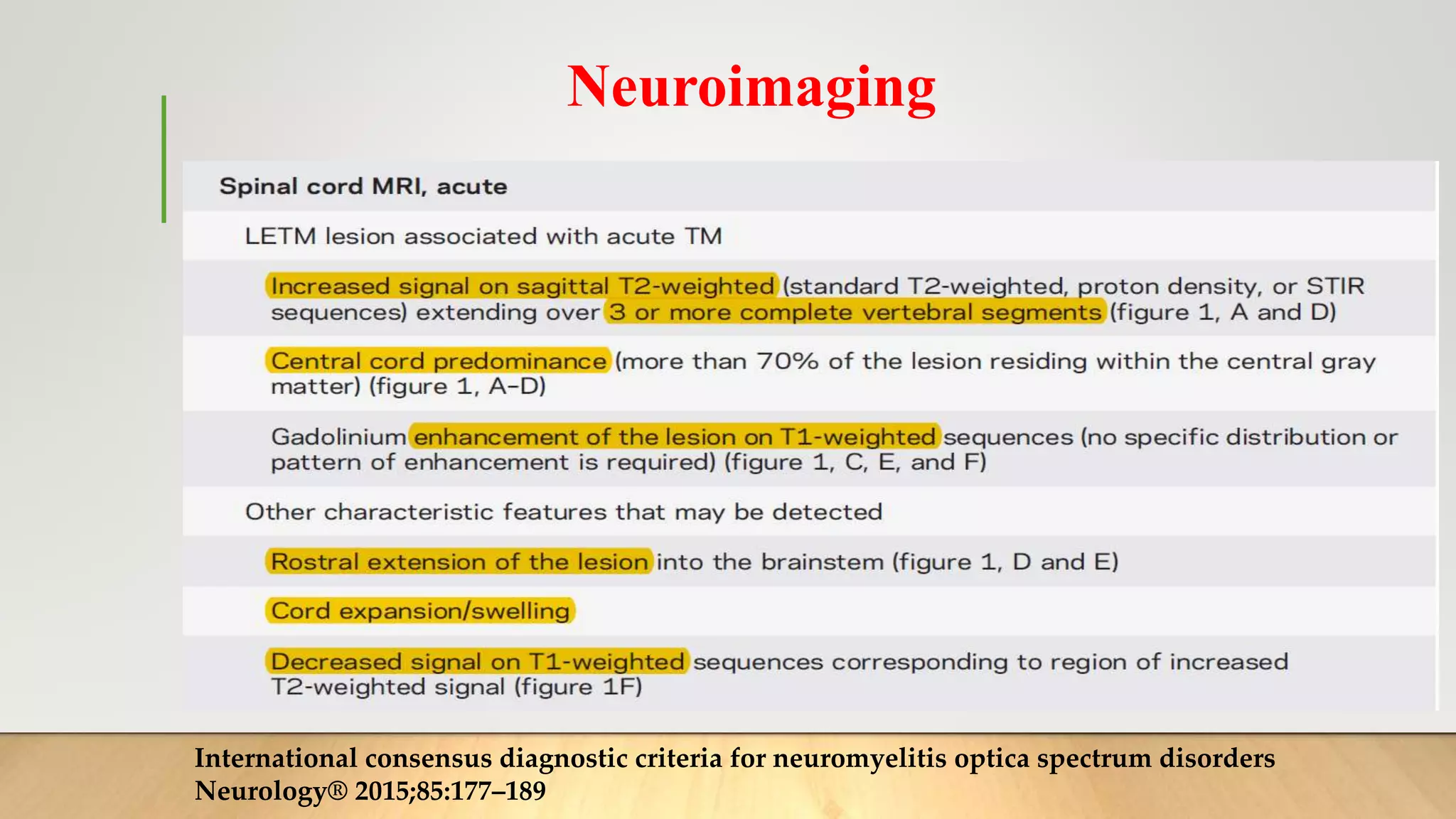
NeuroMyelitis Optica Spectrum Disorder (NMOSD) is an inflammatory disorder of the central nervous system characterized by demyelination and damage of the optic nerves and spinal cord. It was previously considered a variant of multiple sclerosis but is now recognized as a distinct condition mediated by autoantibodies against aquaporin-4. NMOSD can present with optic neuritis causing vision loss or transverse myelitis with varying degrees of weakness and sensory loss. Brain involvement is also seen in around half of patients. The disease predominantly affects women and typically involves recurrent, severe attacks with varying recovery. Diagnosis involves identifying clinical features, MRI imaging, and serologic testing for aquaporin-4 antibodies.