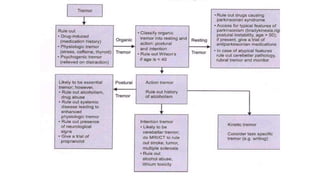
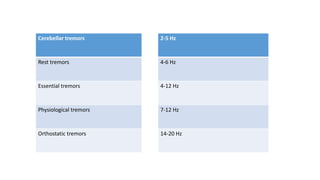
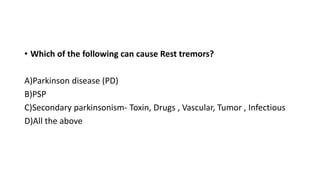
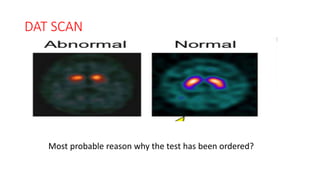
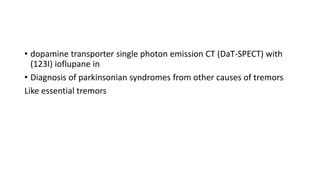
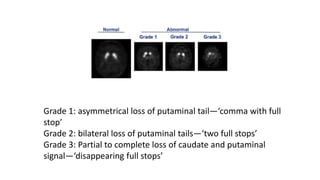
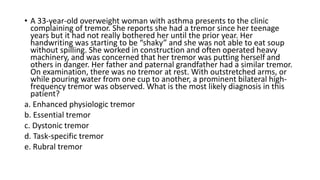
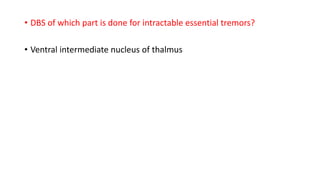
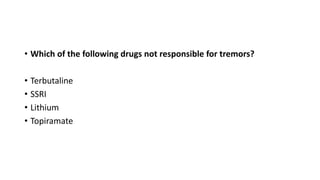
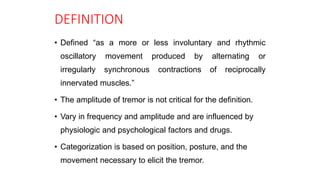
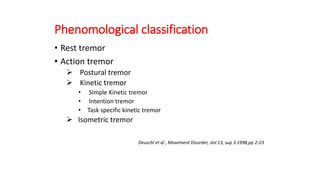
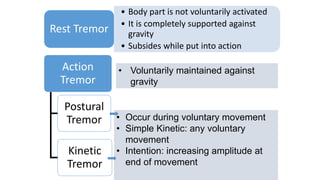
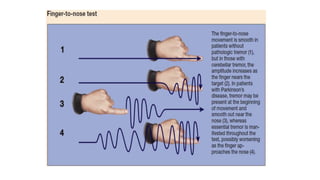
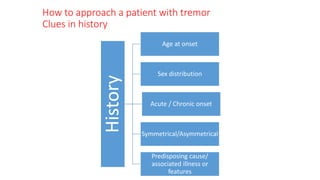
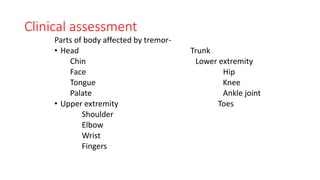
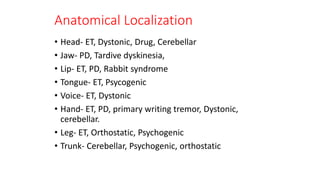
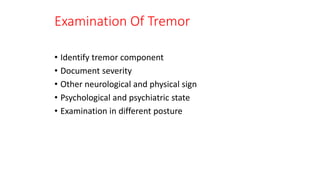
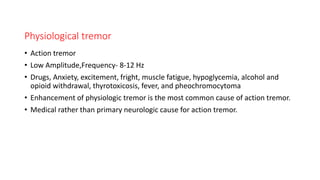
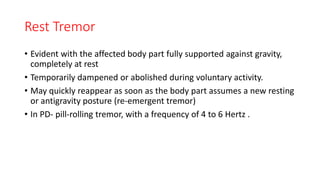
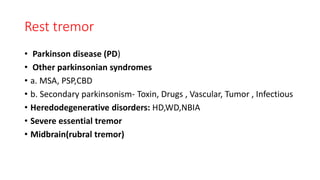
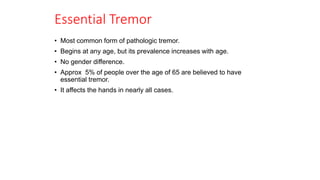
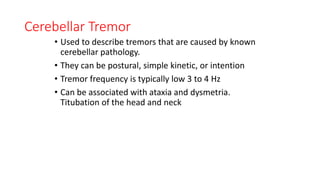
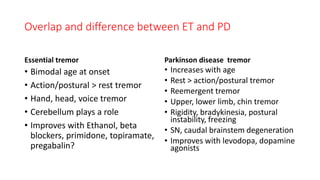
This document discusses the approach to tremors. It defines tremors and classifies them based on frequency, phenomenology, distribution, and etiology. Tremors can be rest tremors, action tremors such as postural tremors and kinetic tremors. Essential tremor is the most common cause of pathological tremor. Parkinson's disease causes rest tremors. Cerebellar tremors have a low frequency. Evaluation of tremors involves history, examination of affected body parts, tremor characteristics, and investigations like MRI and DAT scan to identify the underlying cause. Treatment depends on the cause but may include medications, botulinum toxin injections, or deep brain stimulation.



![Lab Investigations
• Thyroid function tests
• S. ceruloplasmin, S. Cu &24-h urine copper
• Toxic sceen
Imaging
• MRI brain
• TRODAT SPECT
• [18F]-labeled L-3,4-dihydroxiphenylalanine PET is
the best diagnostic modality differentiate it from
other Parkinsonian syndromes as well as ET](https://image.slidesharecdn.com/approachtotremors-200519015448/85/Approach-to-tremors-30-320.jpg)