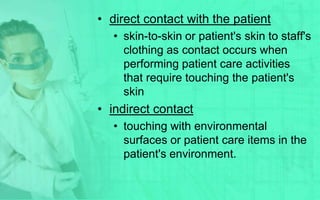
This document outlines transmission-based precaution techniques, including airborne, droplet, and contact precautions. Airborne precautions are for diseases transmitted through small particles that remain suspended in the air, like measles or tuberculosis, and involve respiratory protection, negative pressure rooms, and appropriate ventilation. Droplet precautions are for diseases transmitted through large respiratory droplets, like influenza, and involve masks within 3 feet and private rooms. Contact precautions are for diseases transmitted through direct or indirect contact and involve private rooms, dedicated or disposable equipment, gloves, and hand hygiene.









![• Examples :
• Methicillin (oxacillin)-resistant
Staphylococcus aureus (MRSA
[ORSA])
• Vancomycin-resistant Enterococcus.
• Vancomycin-intermediate-resistant S.
aureus, also known as glycopeptide-
resistant S. aureus.
• Clostridium difficile (when patient has
diarrhea).
• For diapered or incontinent patients,
Escherichia coli 0157:H7, shigella,
hepatitis A, rotavirus.](https://image.slidesharecdn.com/transmission-basedprecautiontechniques-120321080235-phpapp01/85/Transmission-based-precaution-techniques-17-320.jpg)