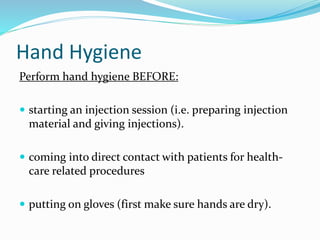
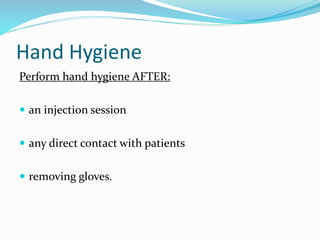
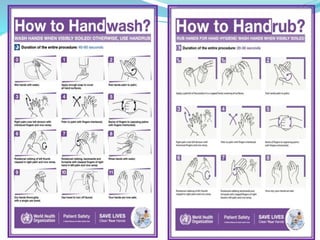
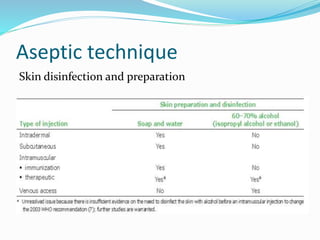
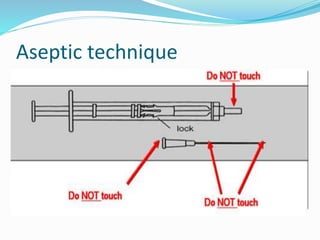
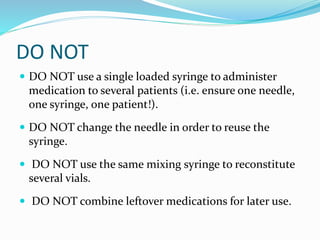
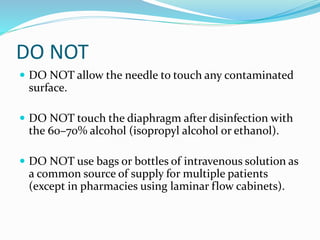
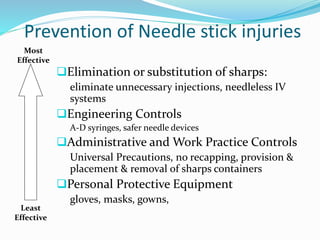
The document outlines the principles of safe injections to prevent harm to patients and healthcare providers, emphasizing the necessity of standard precautions in healthcare settings. It highlights the risks associated with unsafe injection practices, including the transmission of blood-borne pathogens, and proposes prevention strategies such as vaccination of health workers and strict adherence to best practices in hand hygiene, personnel protective equipment, and waste management. Key recommendations include the use of single-use devices, proper disposal of sharps, and avoiding contamination through careful aseptic techniques.