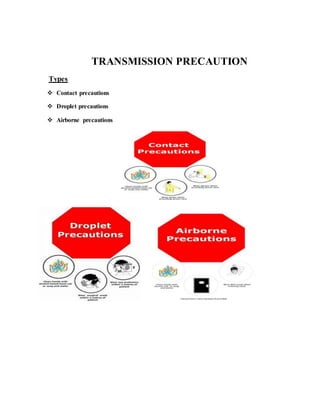
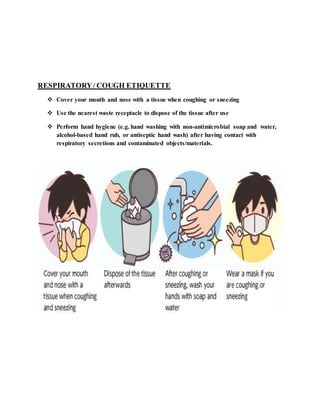
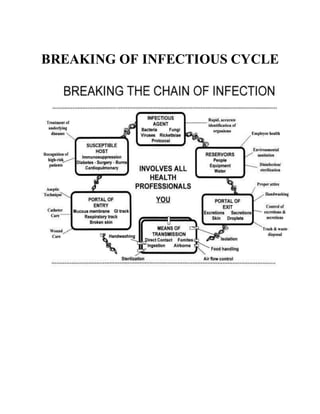
Surgical asepsis refers to procedures used to keep objects and areas completely free from microorganisms. It aims to eliminate both pathogenic and nonpathogenic microbes. Standard precautions like hand hygiene, personal protective equipment, and respiratory etiquette are used to reduce disease transmission. Proper aseptic techniques like sterile fields, principles of asepsis, and transmission-based precautions help maintain sterility and interrupt infection pathways.