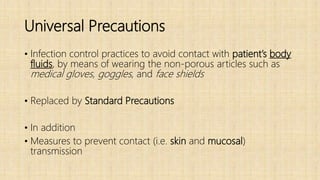
This document provides an overview of standard precautions and infection control procedures for a hospital induction training. It discusses standard precautions including hand hygiene, personal protective equipment, environmental cleaning, and respiratory etiquette. It also covers biomedical waste management, safe injection practices including needlestick injury management, and spill management procedures. The goal is to educate new hospital staff on universal safety protocols to prevent the transmission of infectious diseases.