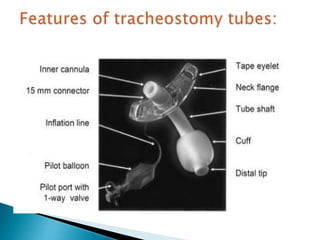
A 50-year-old female patient was admitted to the ICU with a spontaneous intracranial hemorrhage and underwent a tracheostomy after 7 days. After 4 days, the outer part of the tracheostomy tube became longer for no apparent reason. The patient then developed surgical emphysema, hypoxia, and arrested despite attempts at reintubation. The resident was unable to explain what happened to the tracheostomy tube.