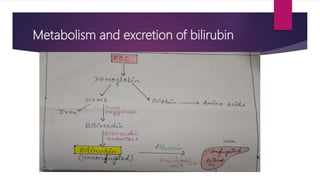
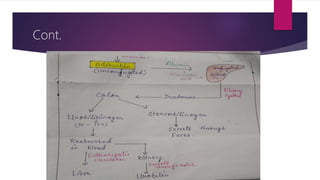
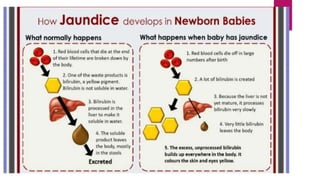
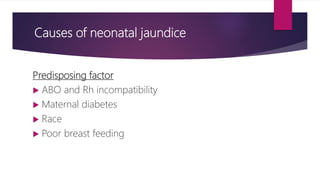
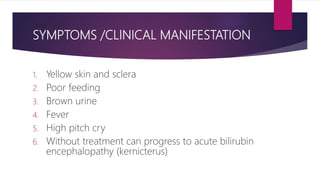
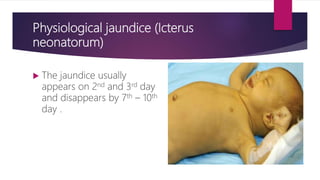
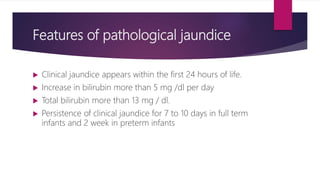
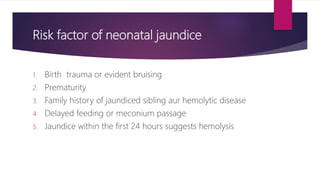
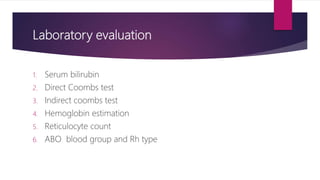
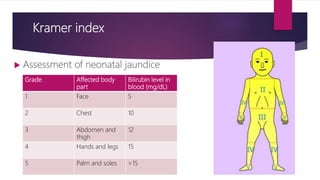
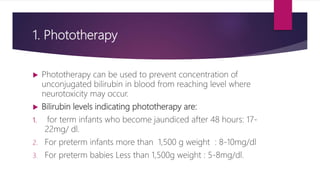
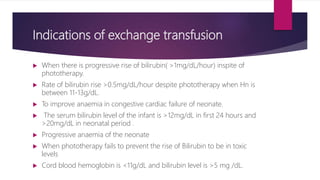
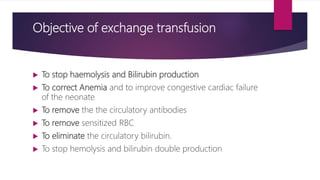
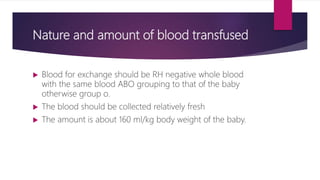
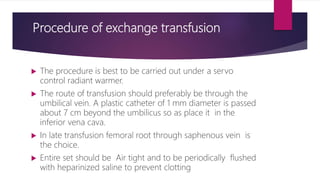
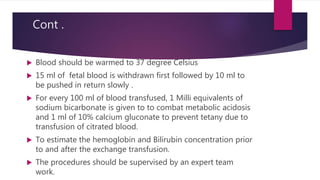
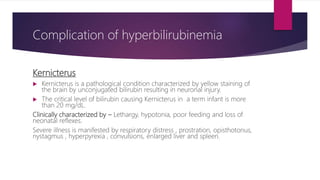
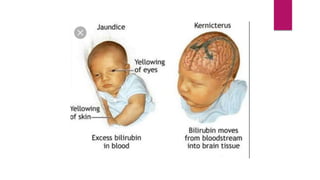
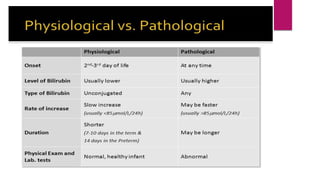
The document discusses neonatal jaundice, characterized by yellow discoloration of a newborn's skin and eyes due to high bilirubin levels. It differentiates between physiological, pathological, and breast milk jaundice, including their causes, symptoms, laboratory evaluations, and treatment options. Management strategies include phototherapy, pharmacological therapy, and exchange transfusion, with an emphasis on prevention and monitoring for complications such as kernicterus.