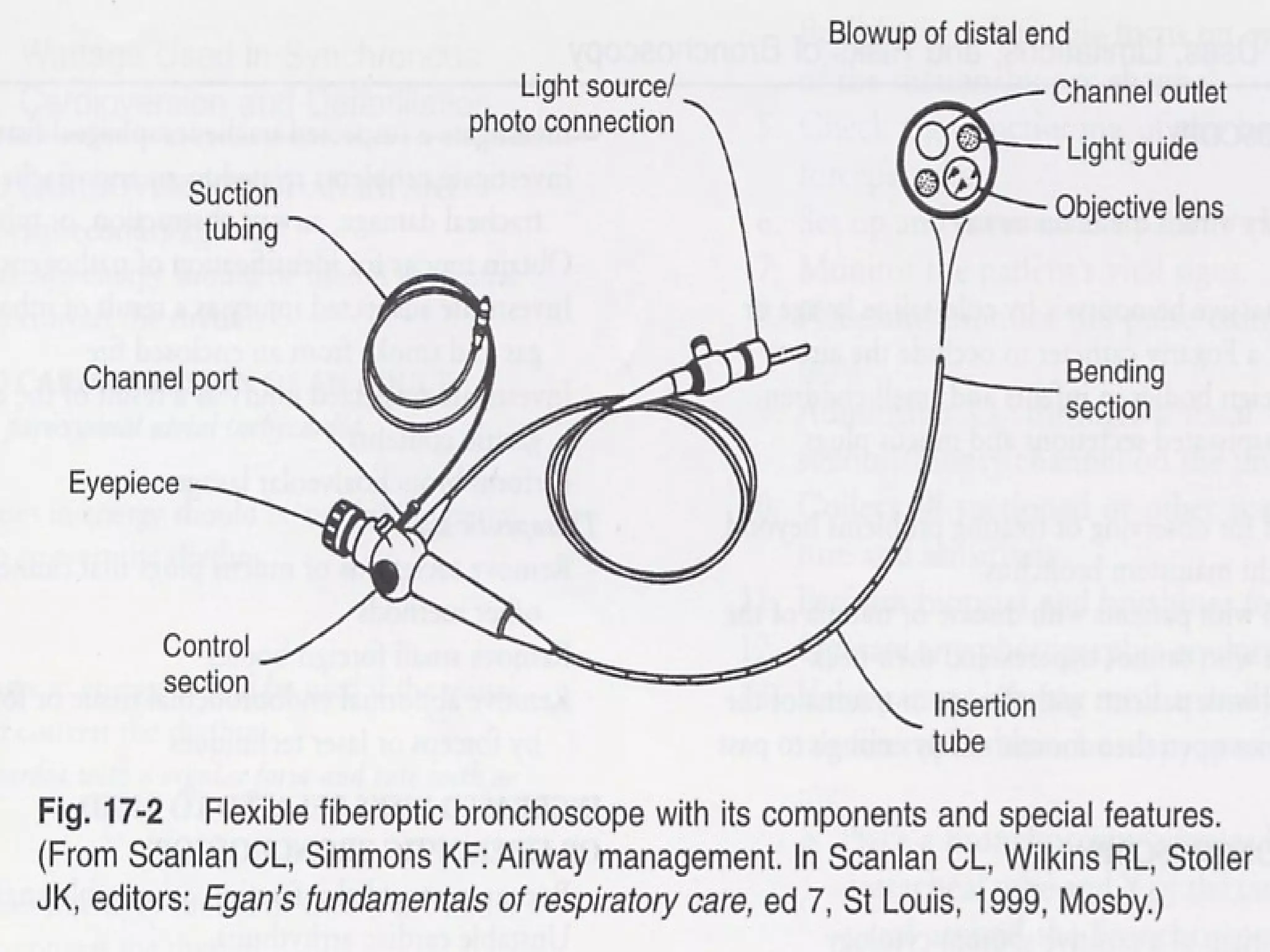
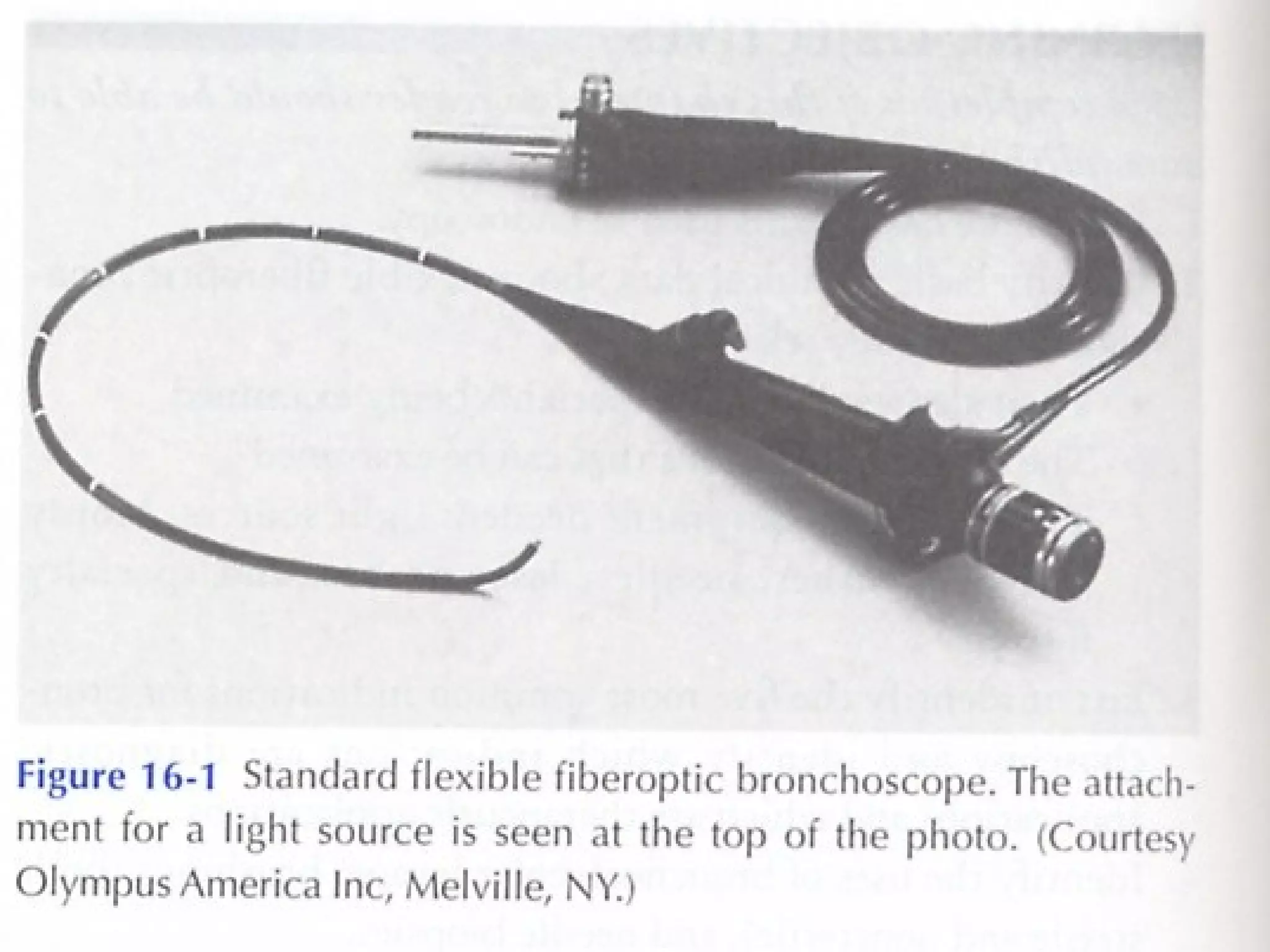
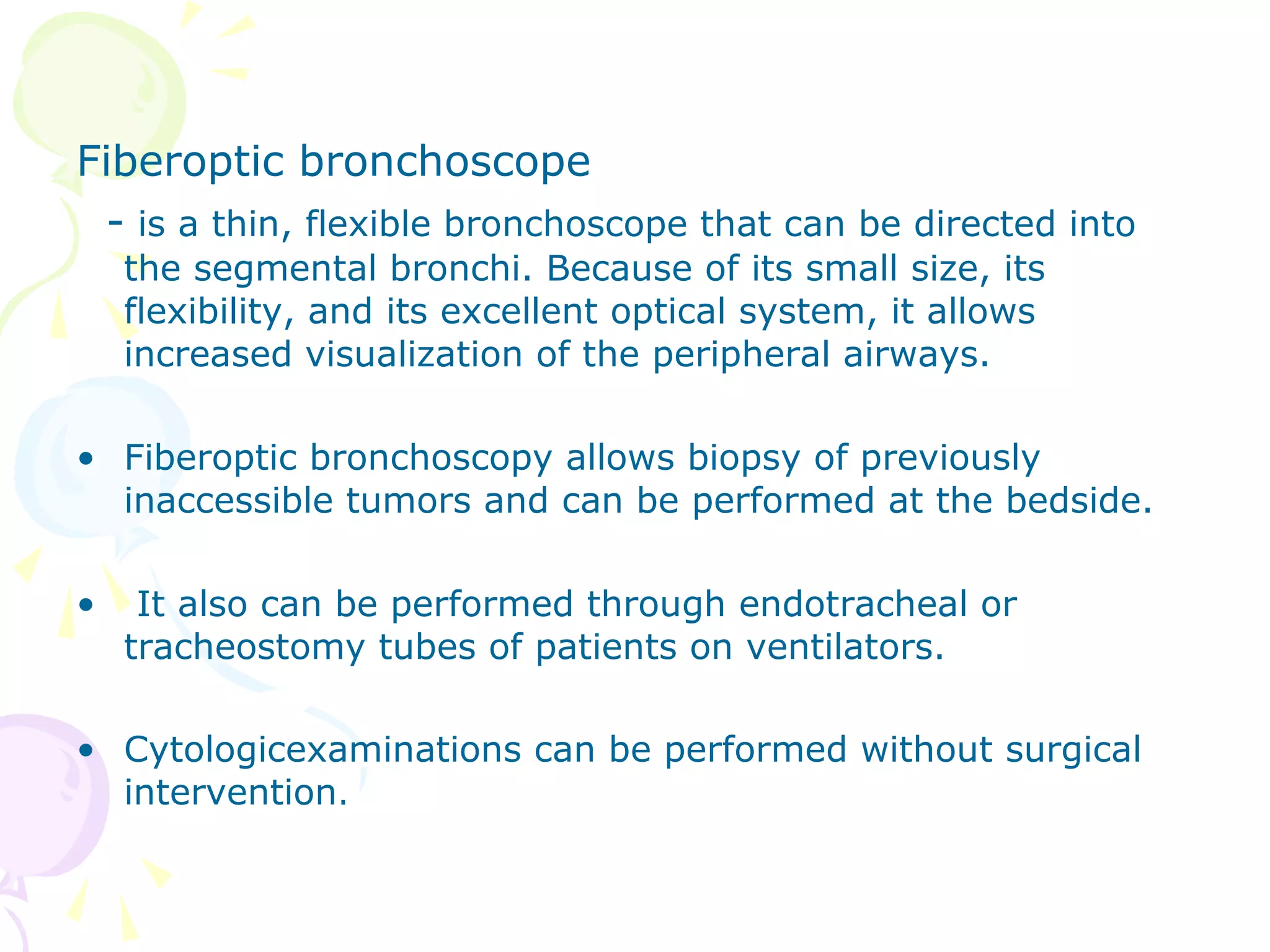
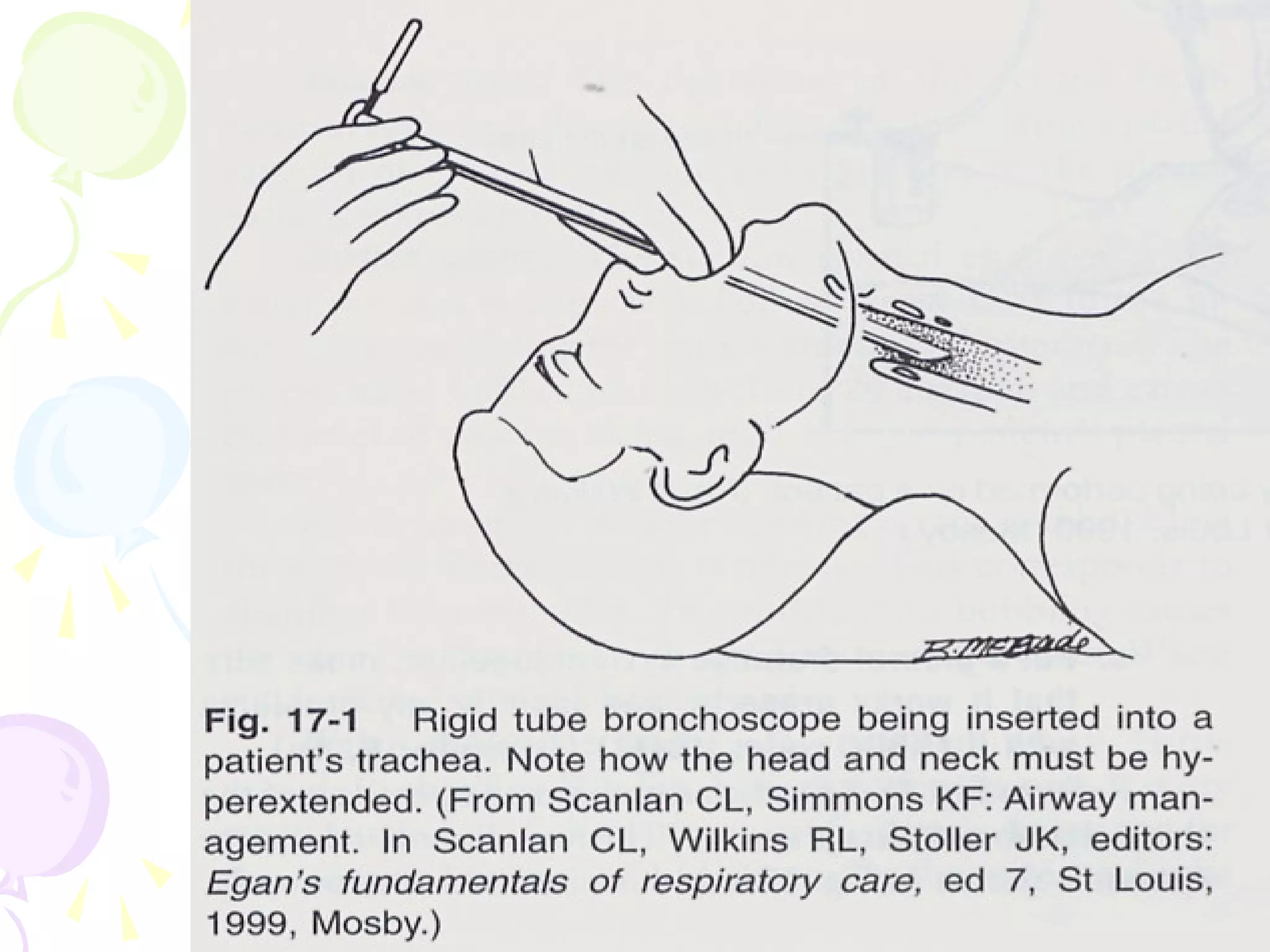
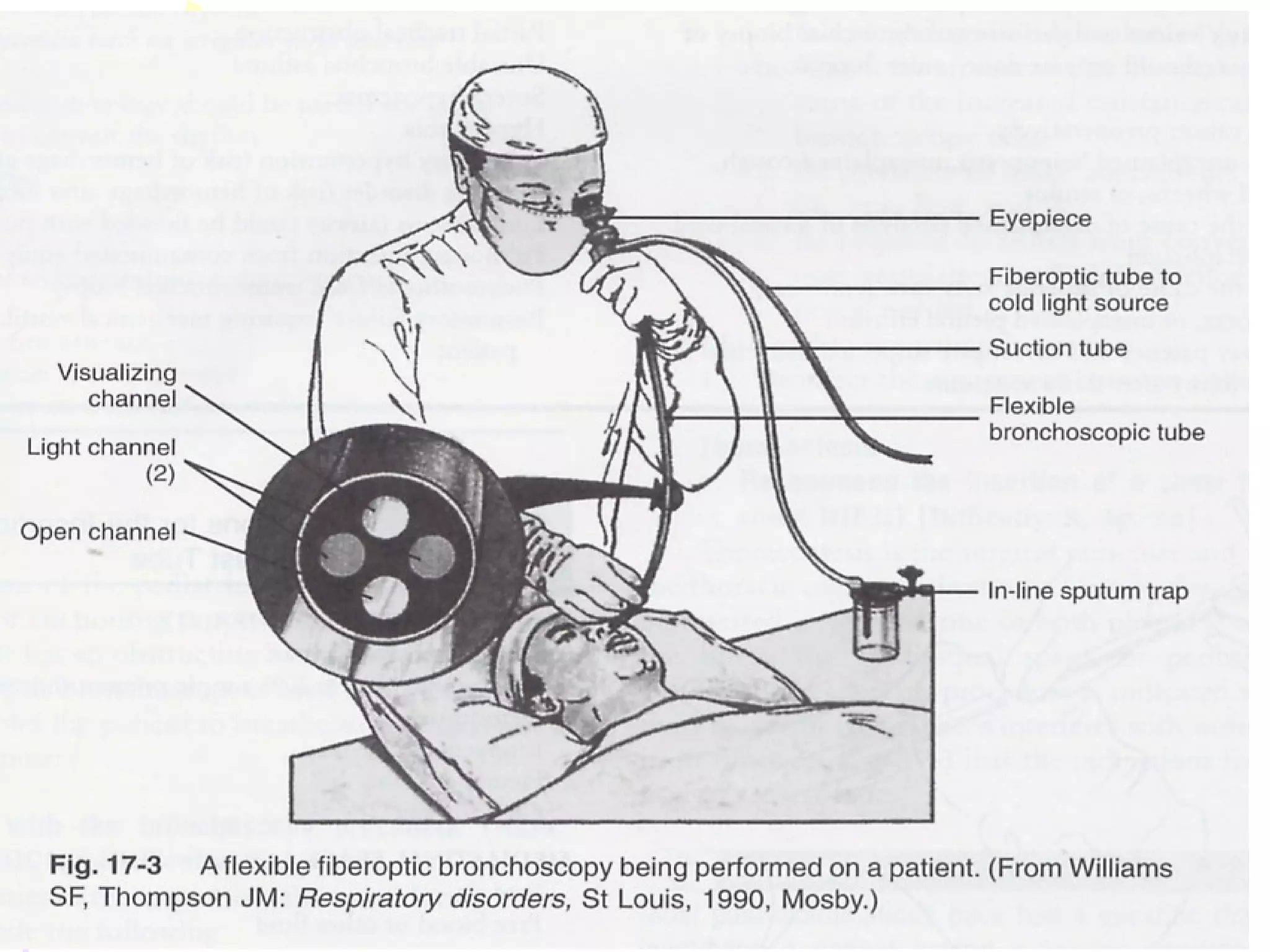
Bronchoscopy is a procedure used for direct examination of the airways, primarily utilizing flexible fiberoptic or rigid bronchoscopes. It serves both diagnostic purposes, such as tumor assessment and bleeding site identification, and therapeutic roles, including foreign body removal and secretion clearing. Pre- and post-procedure care is essential, with potential hazards such as bleeding, bronchospasm, and aspiration involved.