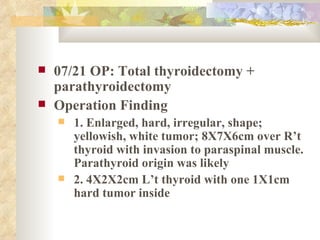
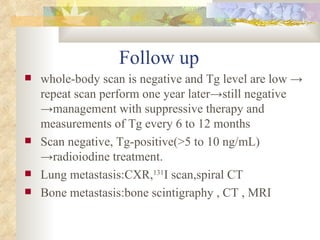
1. The patient has a history of thyroid cancer with metastases to the lungs and skull, and underwent total thyroidectomy and parathyroidectomy.
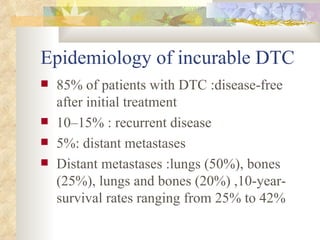
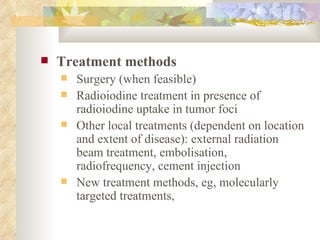
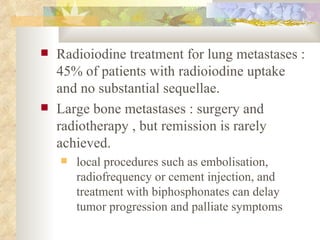
2. Treatment options for recurrent or metastatic thyroid cancer include radioactive iodine treatment, surgery, external beam radiation, and molecularly targeted therapies.
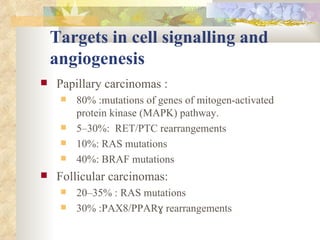
3. Molecular targeted therapies that show promise for thyroid cancer work by inhibiting pathways involved in cell signaling and angiogenesis, such as the MAPK and PI3K pathways, or by restoring radioiodine uptake.
![Recurrent disease in the thyroid bed or in other soft tissue, or aerodigestive tract -> staging with endoscopies and various imaging modalities Disease limited to the neck :extensive surgery and external-beam radiotherapy patients older than 40 years , poorly-differentiated tumors, no radioiodine uptake, large tumor burden, rapid progressive disease, soft tissue involvement, and high [18F]FDG uptake : develop distant metastases after treatment .](https://image.slidesharecdn.com/2657136/85/Thpt-19-320.jpg)
![Treatment of patients with persistent or recurrent disease Indications Abnormal clinical findings Abnormal imaging findings Increasing trend in serum thyroglobulin concentration Staging Neck ultrasonography, whole body scintigraphy with a large activity of radioiodine Conventional imaging: neck and chest CT, bone MRI, [18F]FDG PET Fine-needle biopsy or surgical biopsy in case of unusual presentation](https://image.slidesharecdn.com/2657136/85/Thpt-20-320.jpg)
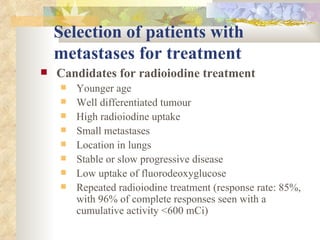
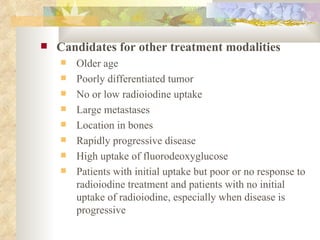
![High initial [18F]FDG uptake : indicate progressive disease and resistance to radioiodine treatment -> can help to select patients who should be treated either with radioiodine or with other modalities Complete remission after treatment: only a third of patients with metastases](https://image.slidesharecdn.com/2657136/85/Thpt-25-320.jpg)