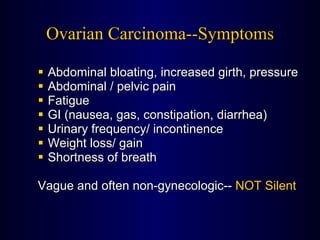
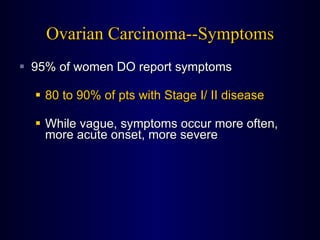
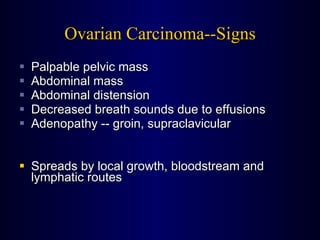
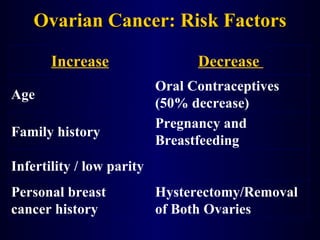
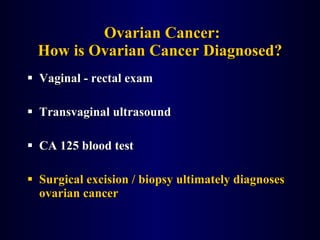
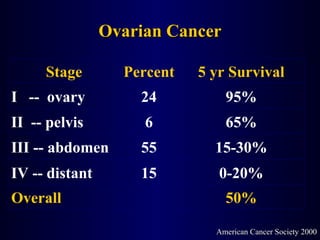
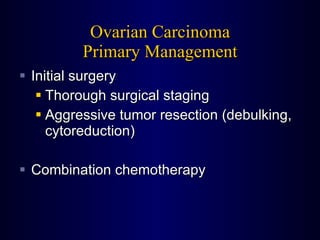
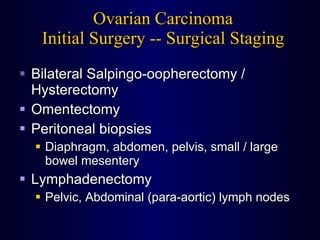
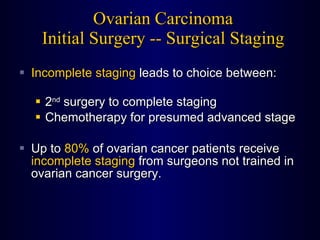
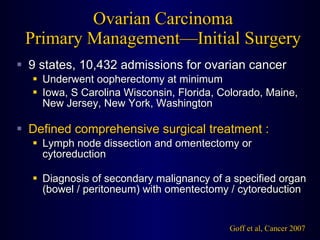
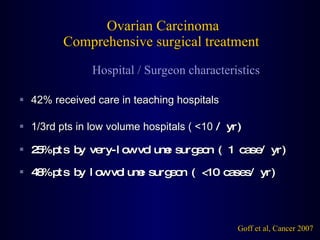
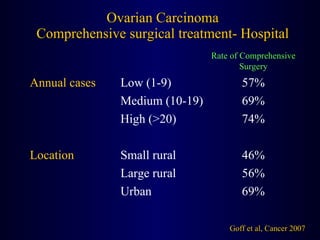
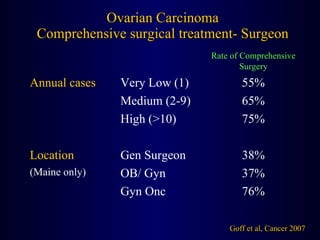
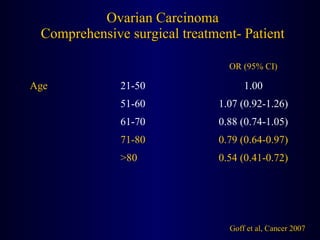
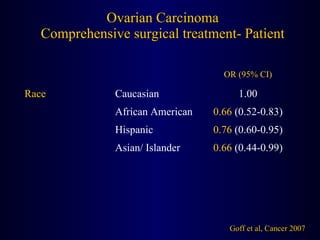
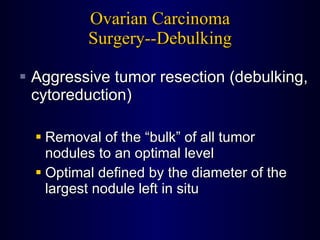
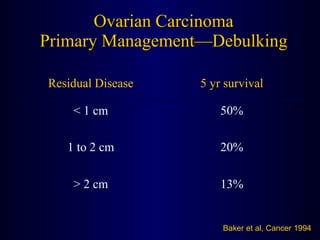
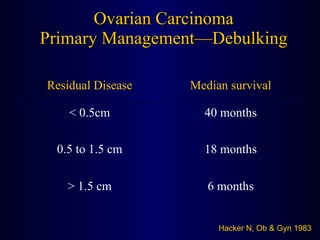
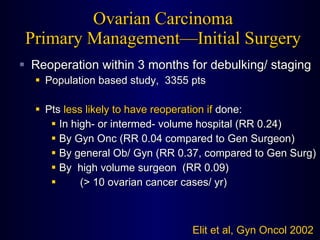
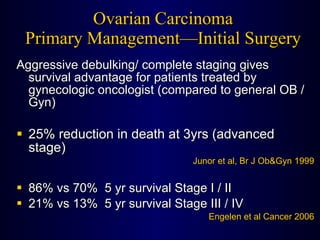
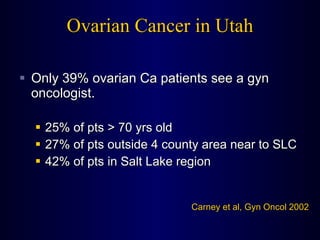
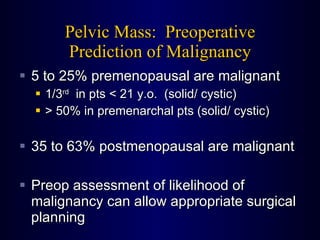
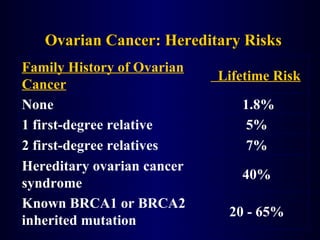
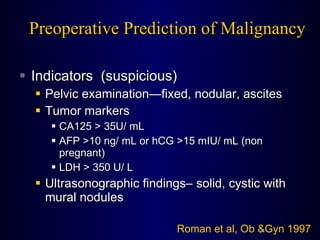
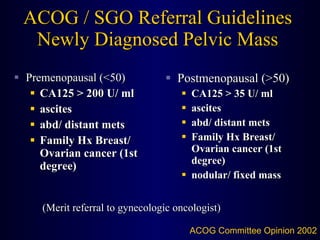
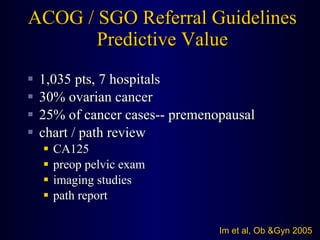
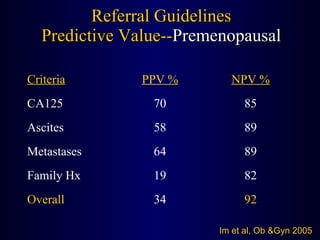
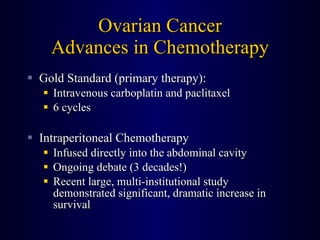
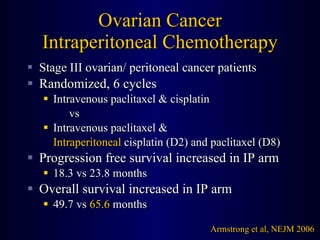
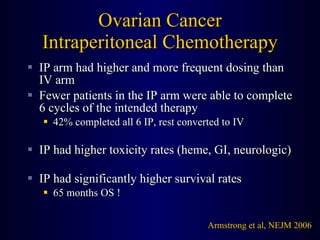
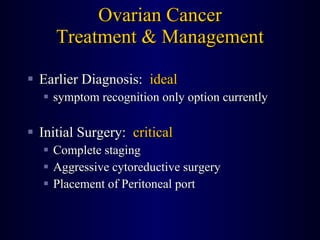
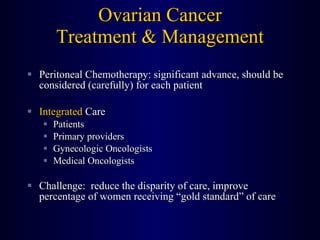
The document discusses ovarian cancer treatment and management. It covers symptoms, risk factors, diagnosis methods, surgical staging and debulking, chemotherapy options including the gold standard of intravenous carboplatin and paclitaxel as well as emerging intraperitoneal chemotherapy showing increased survival. It emphasizes the importance of complete surgical staging and aggressive cytoreductive surgery for optimal outcomes and challenges of ensuring all patients receive standard of care treatment by gynecologic oncologists.