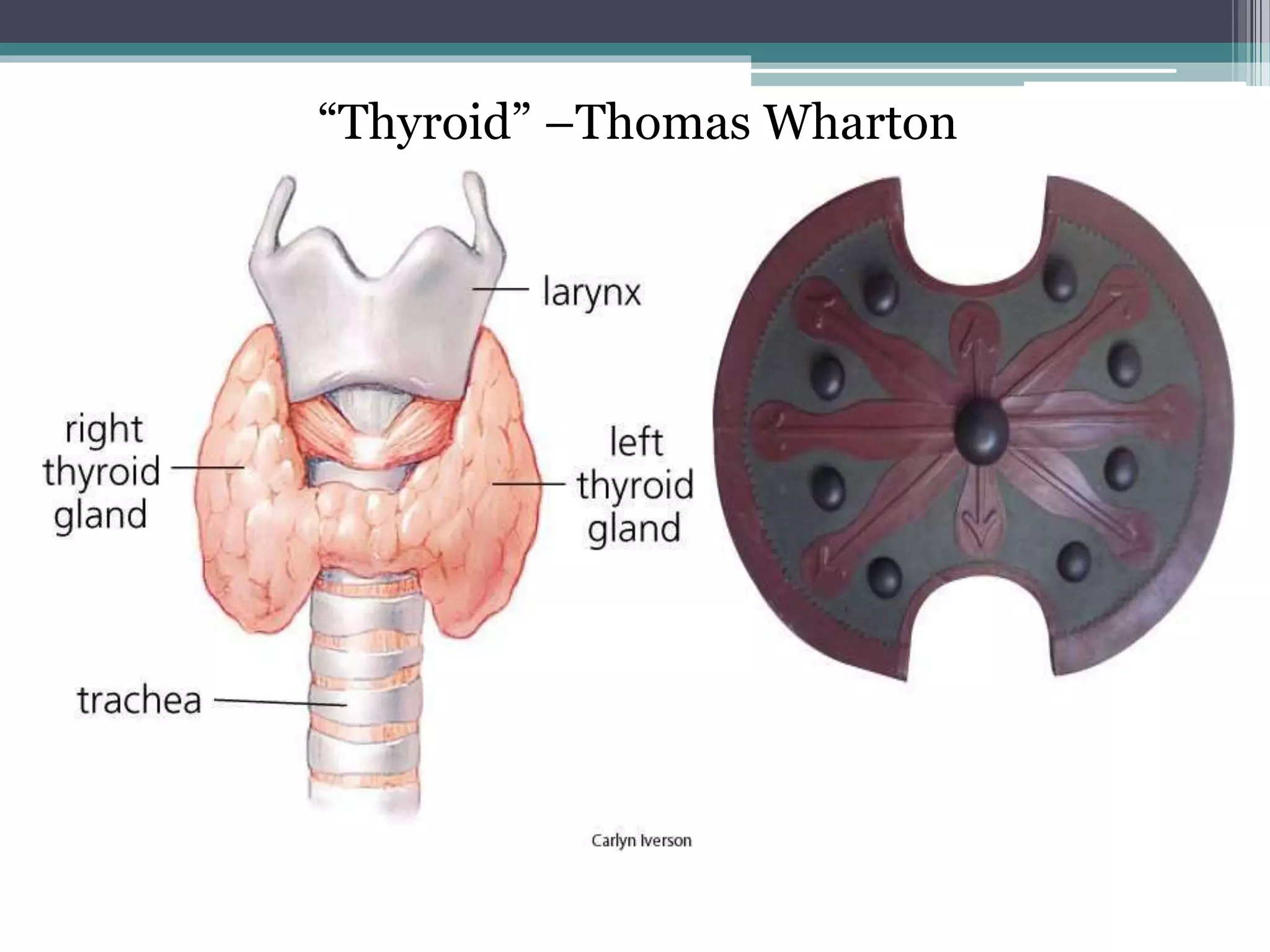
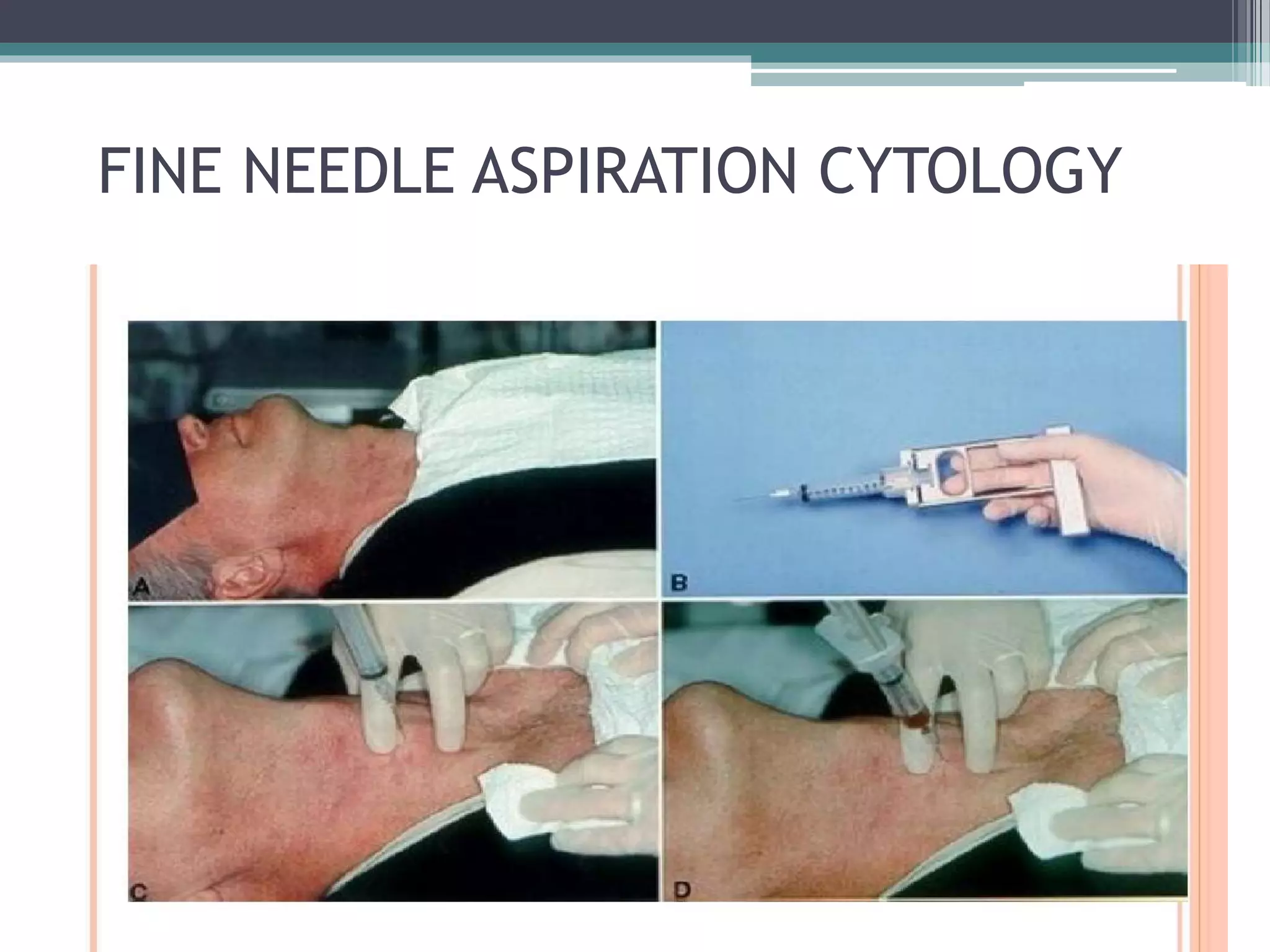
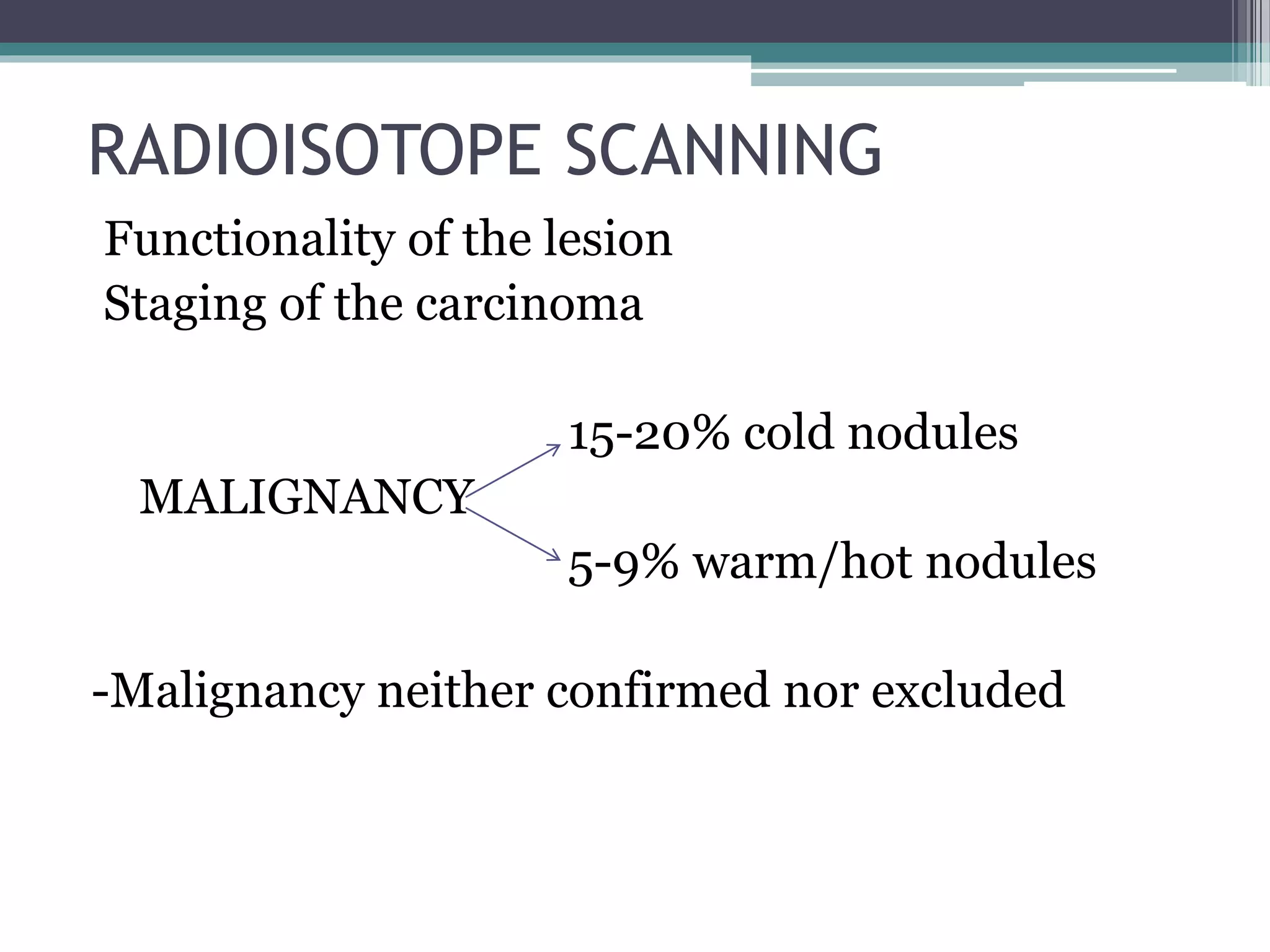
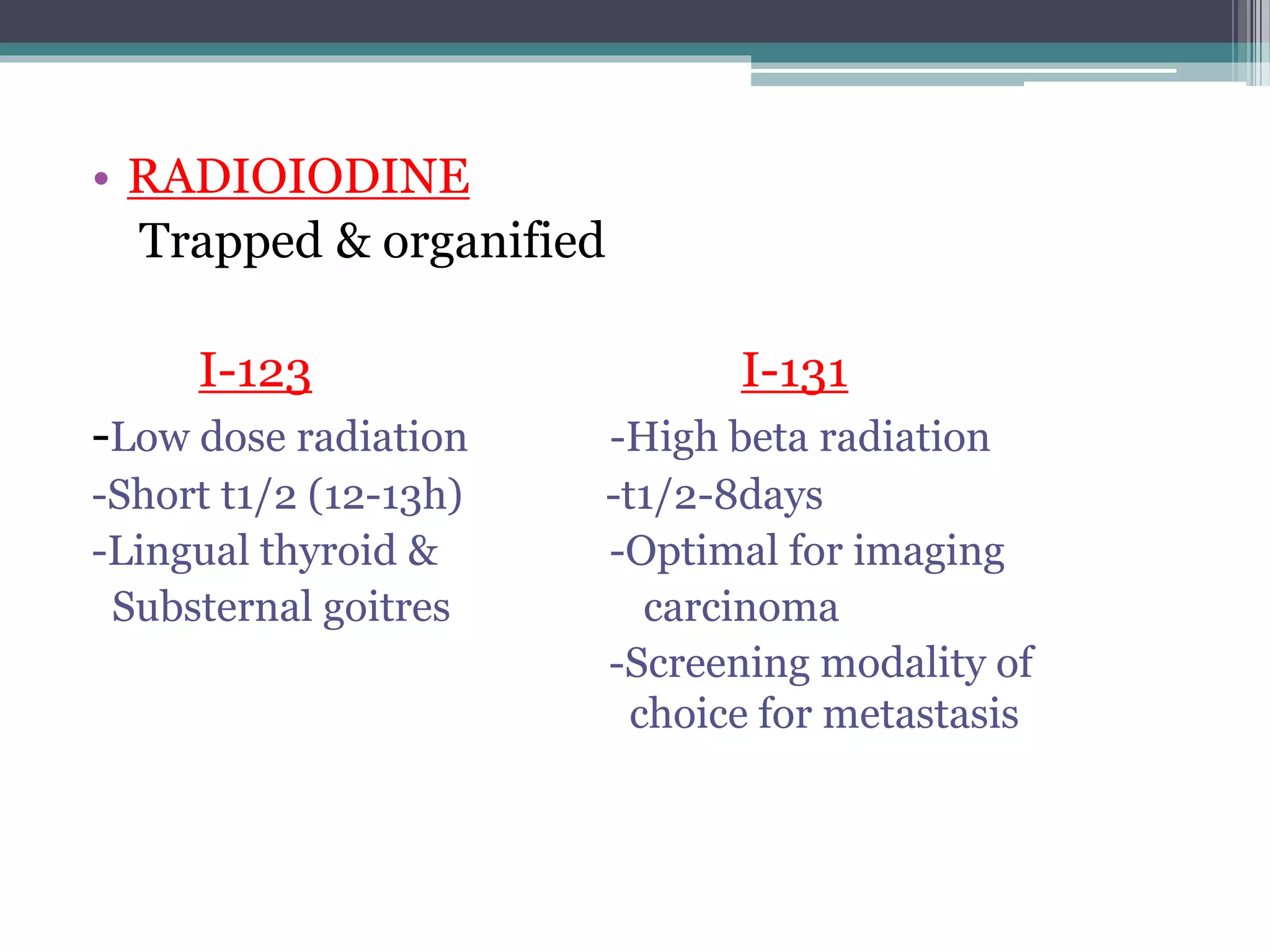
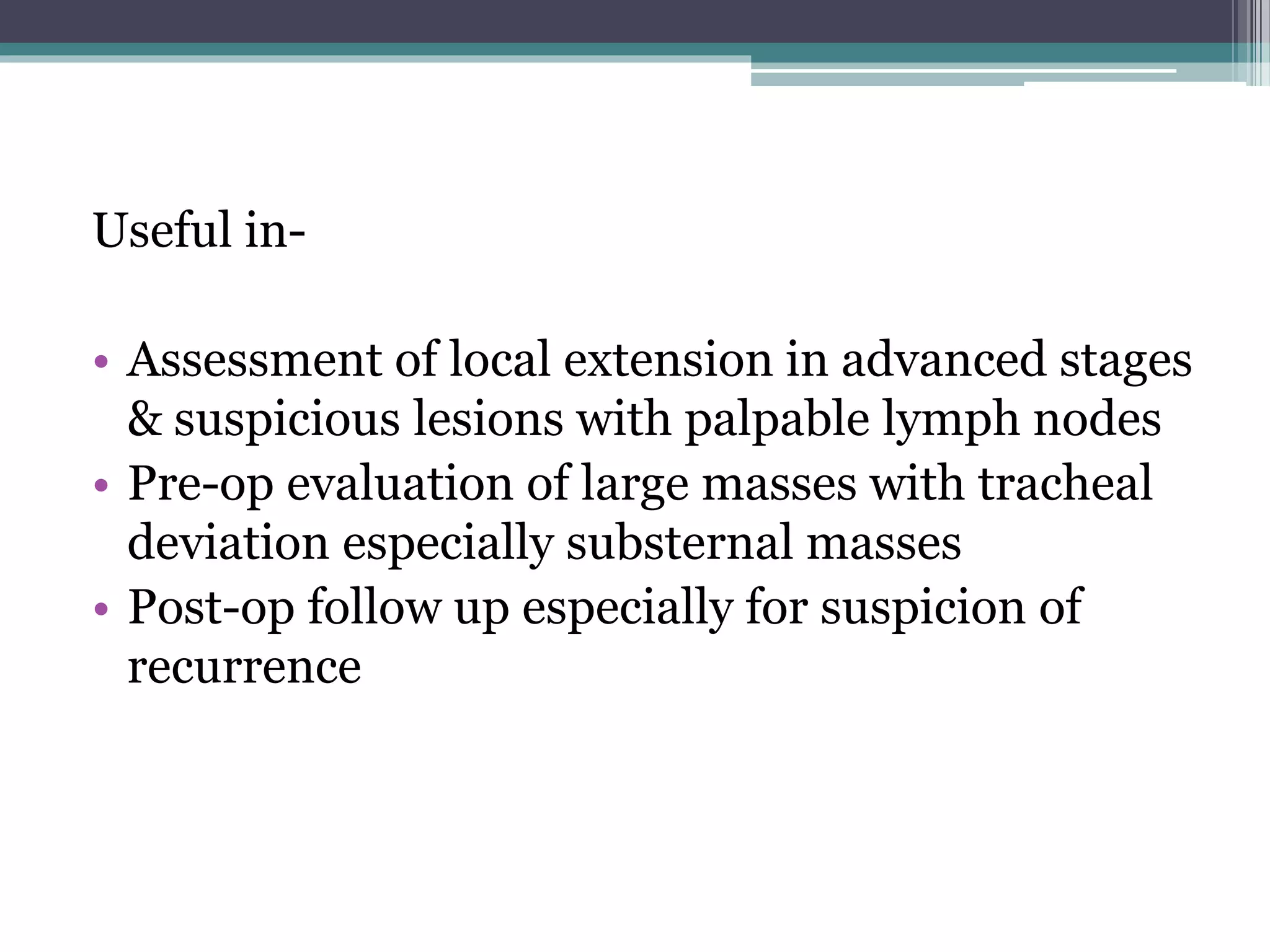
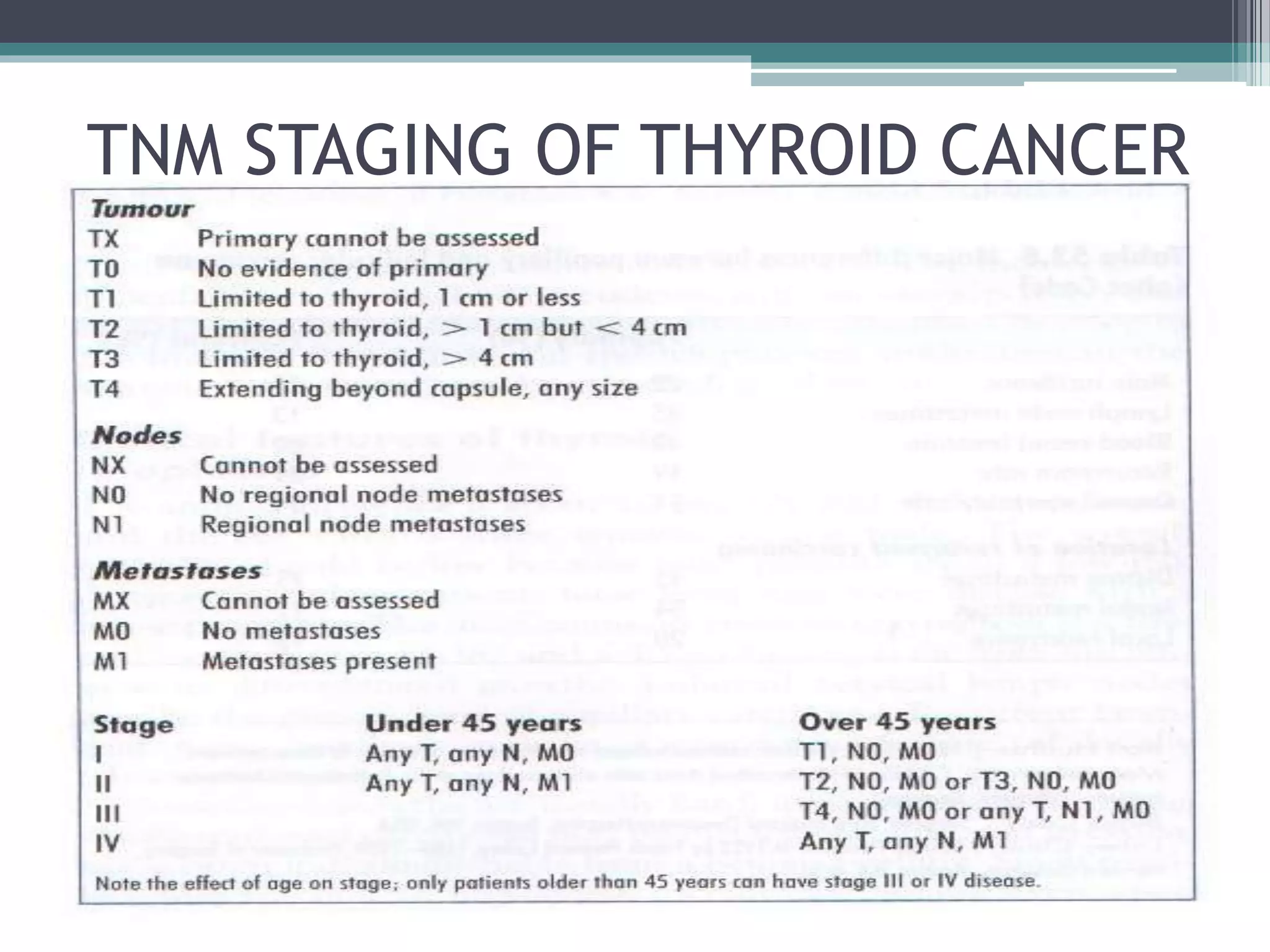
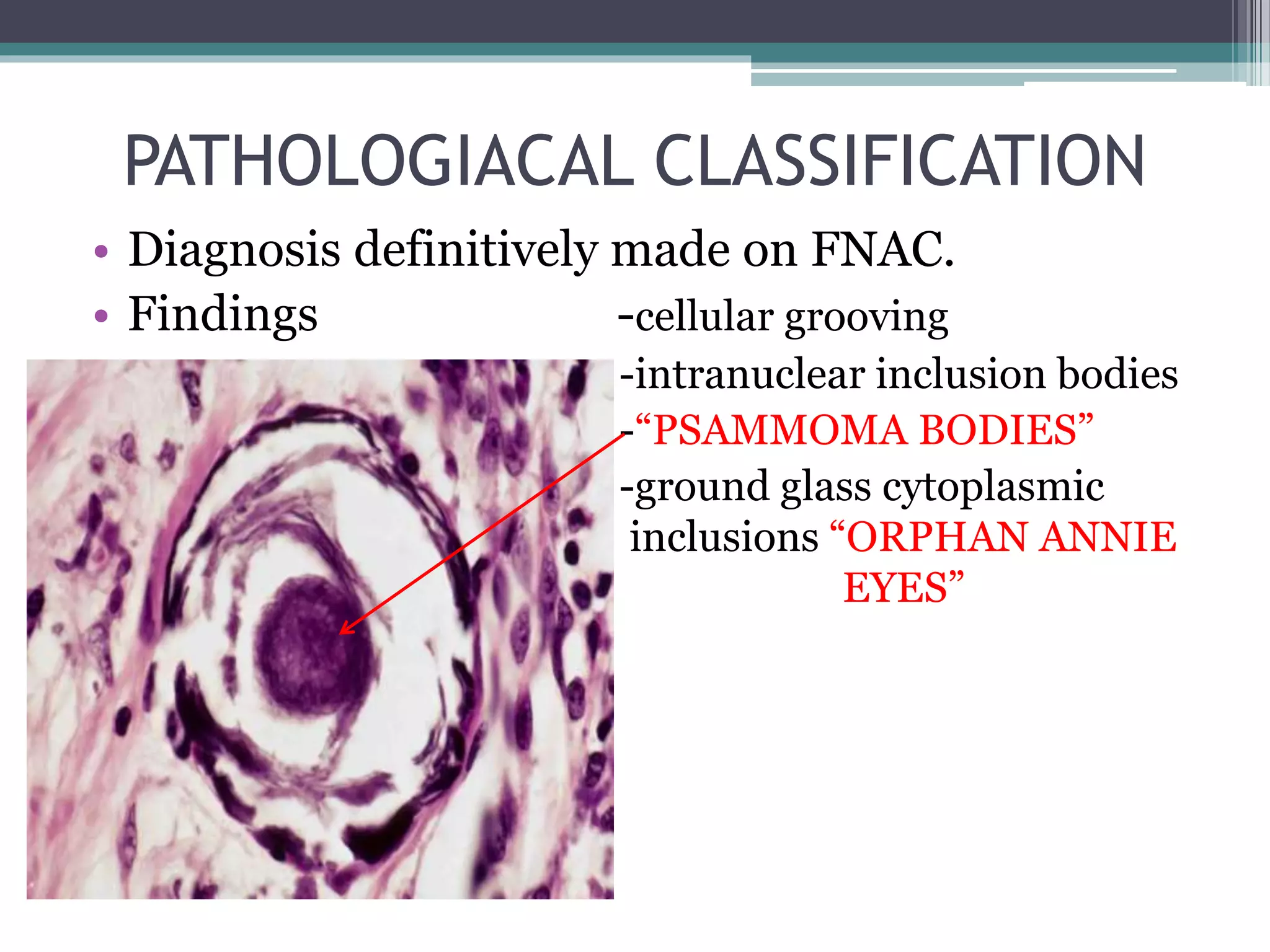
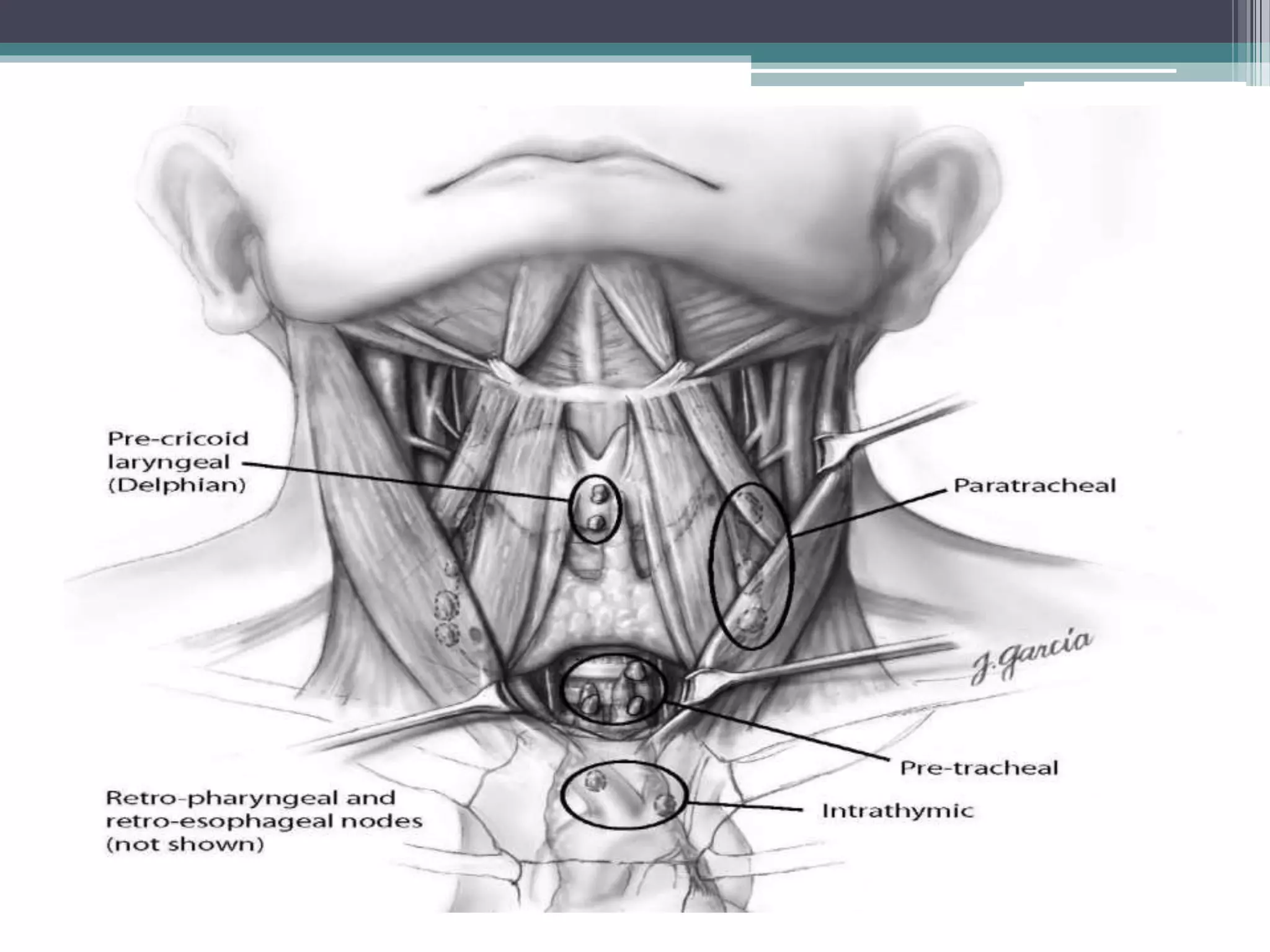
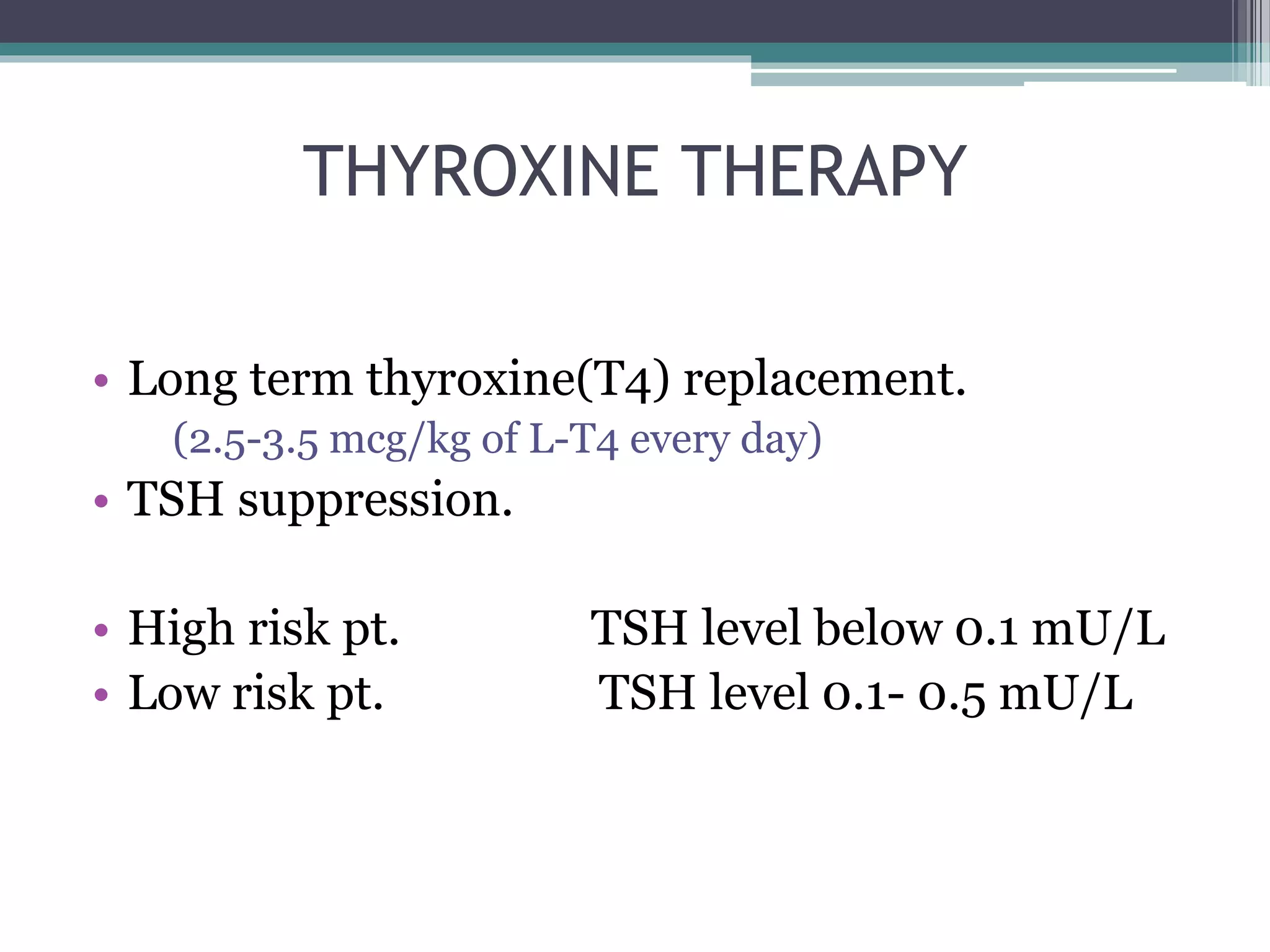
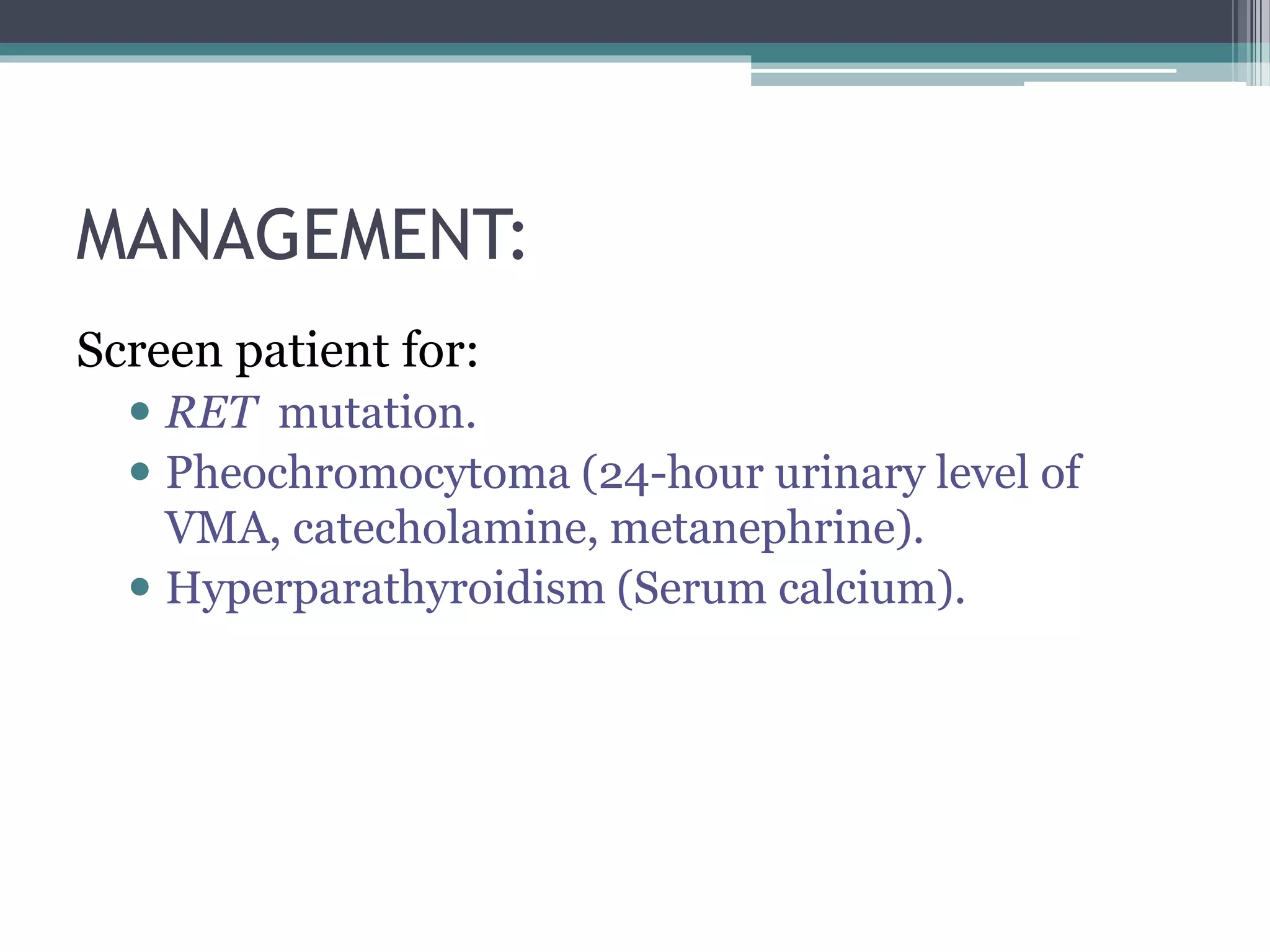
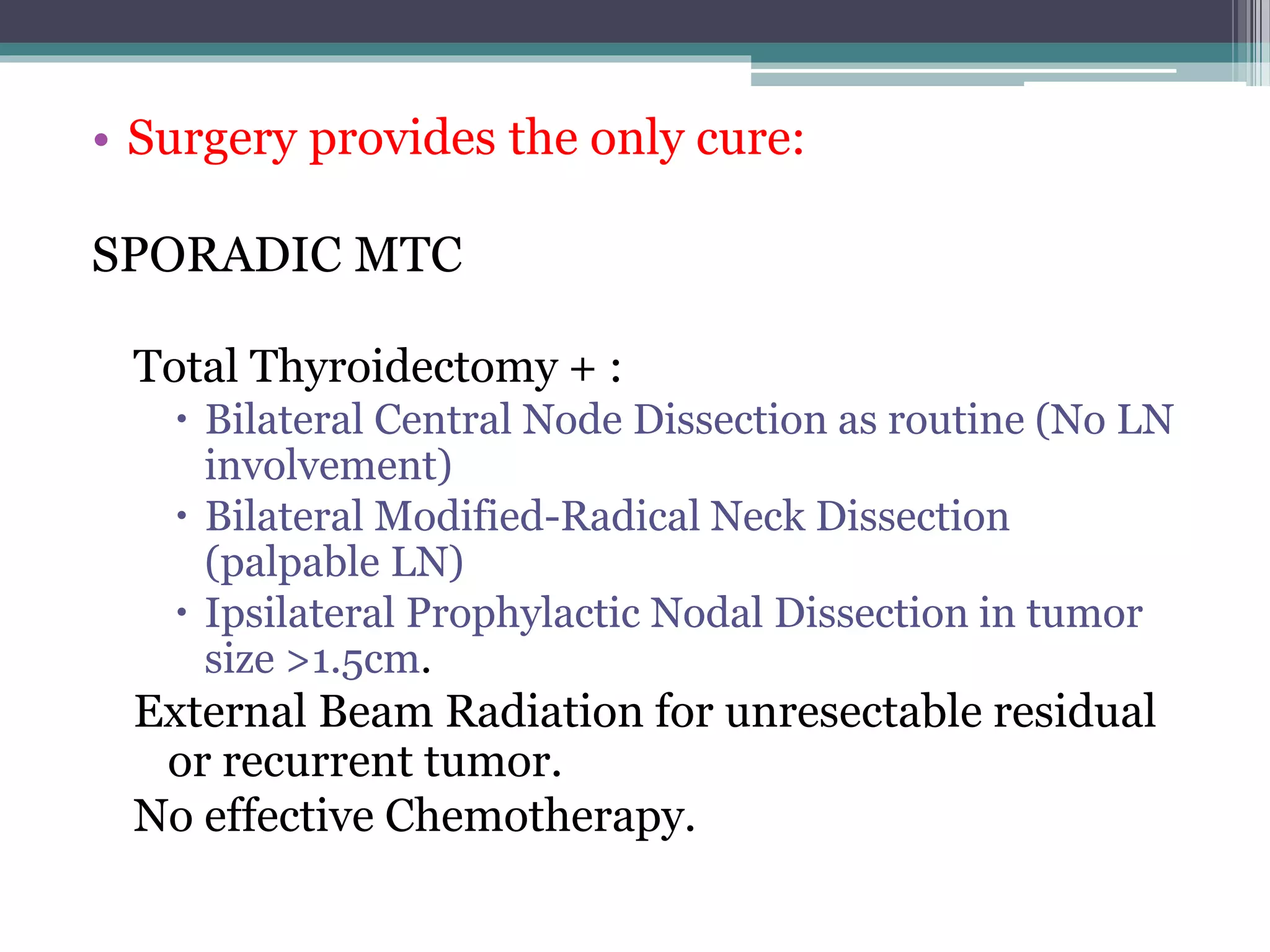
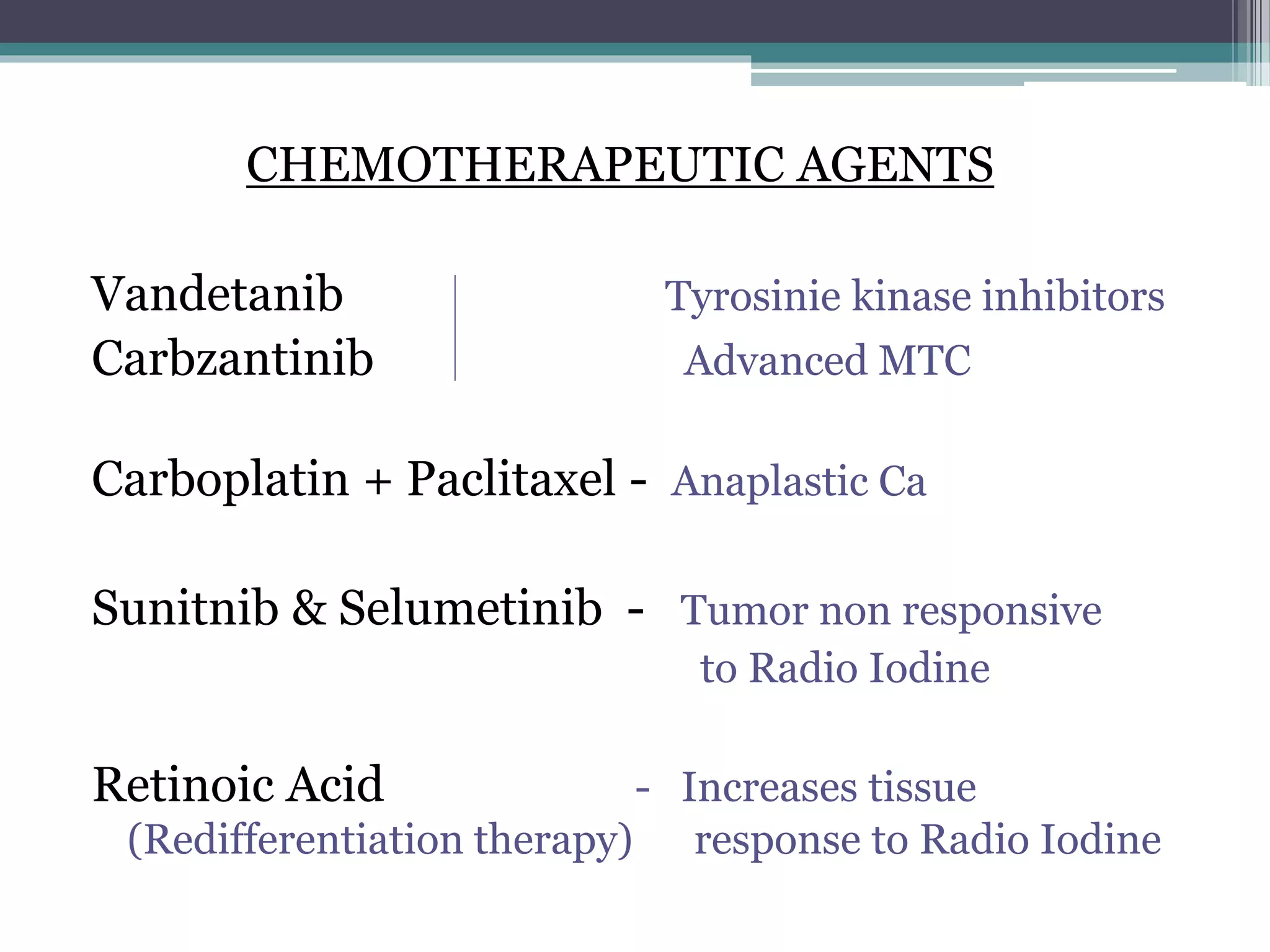
This document provides information on carcinoma of the thyroid gland. It begins with epidemiological data, noting it is the most common endocrine malignancy and incidence has risen in recent decades. Risk factors include radiation exposure, family history, and iodine deficiency. Presentation is typically a painless neck mass. Evaluation involves physical exam, ultrasound, fine needle aspiration, and radioactive iodine scans. Treatment depends on cancer type but generally involves surgery and radioactive iodine therapy. Long-term monitoring of thyroid markers is important for surveillance.