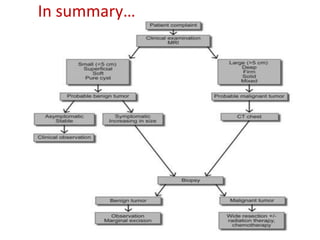
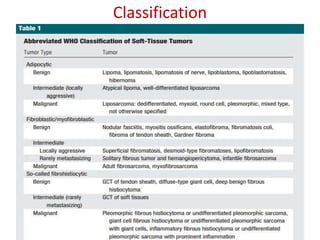
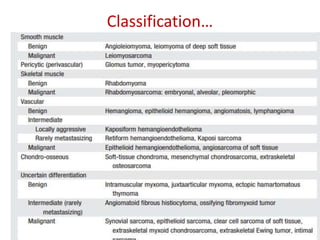
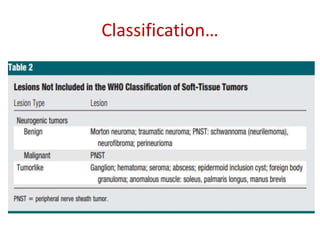
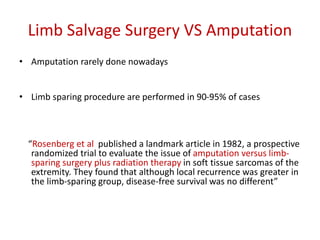
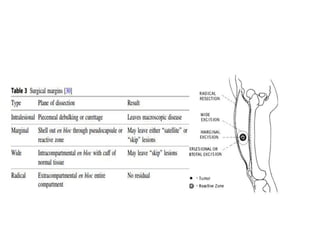
This document provides information about soft tissue tumors. It discusses the epidemiology, classification, etiology, diagnosis and treatment of both benign and malignant soft tissue tumors. Some key points include:
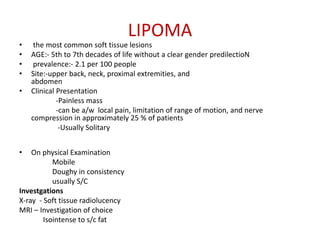
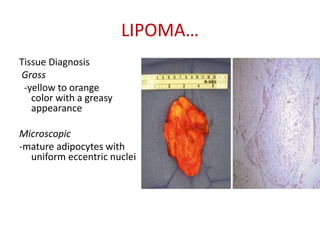
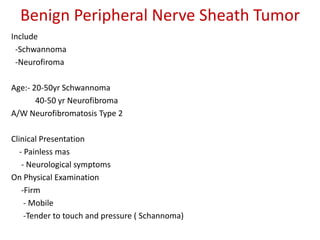
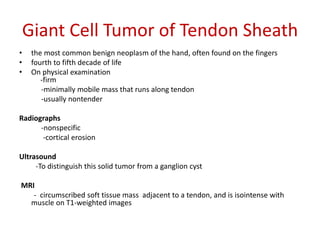
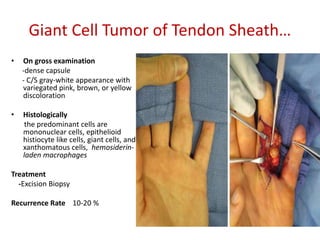
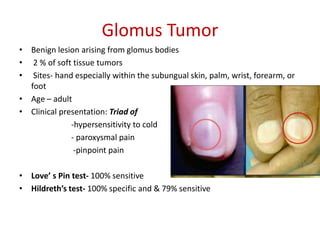
- Benign soft tissue tumors are more common than sarcomas. Common benign tumors include lipomas, schwannomas and giant cell tumors of the tendon sheath.
- Risk factors for soft tissue sarcoma include exposure to herbicides/pesticides, radiation exposure, genetic conditions and viral infections.
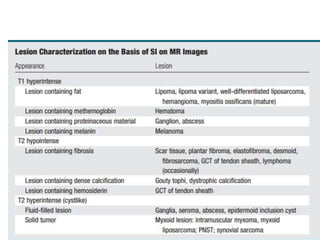
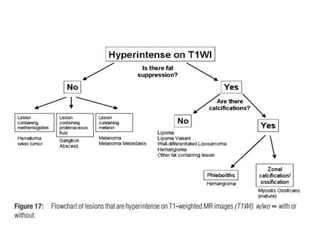
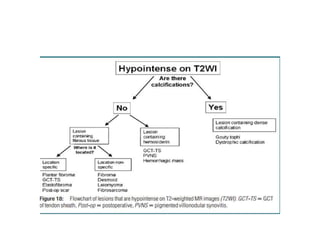
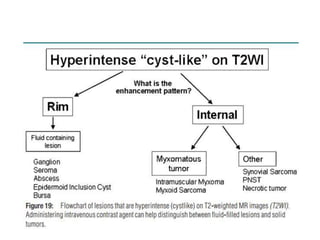
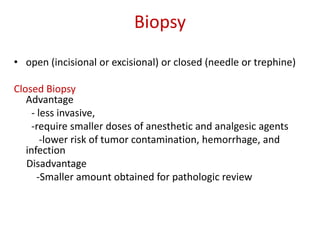
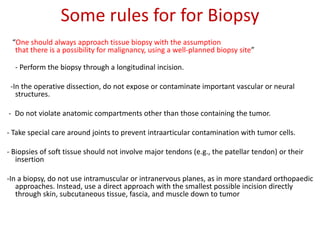
- MRI is usually the best imaging modality for evaluating soft tissue tumors. Biopsy is needed for diagnosis.
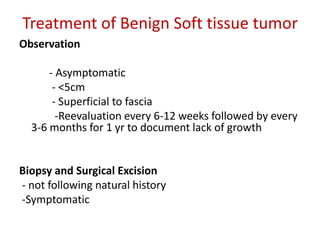
- Treatment depends on whether the tumor is benign or malignant. Benign tumors may
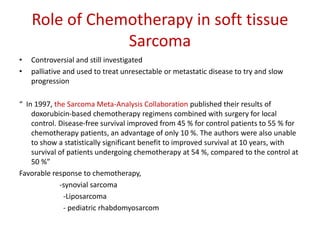
![PET Scan
• assess metabolic function and can be used
to diagnose, stage, and monitor treatment
response for many cancers, and some soft
tissue tumors.
• One specific application is in the evaluation
of multifocal desmoid tumors, and more
specifically, response to treatment.
“ Kasper et al. demonstrated that PET imaging
might complement CT and improve the
assessment of patients with desmoid
tumors. Imatinib, a tyrosine kinase inhibitor,
has been shown to successfully stabilize
desmoid tumors, and PET imaging has been
used to monitor response to imatinib
treatment in patients with multifocal
desmoids [9]”](https://image.slidesharecdn.com/softtissuetumor-160706134441/85/Soft-tissue-tumor-22-320.jpg)
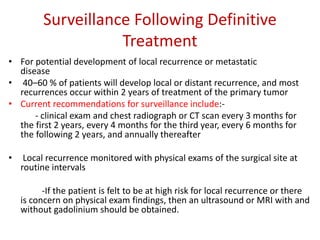
![Role of Radiotherapy in soft tissue
sarcoma
• enhance local control
• preserve function
• achieve acceptable cosmesis by contributing to tissue preservation
“Dagan et al. performed a retrospective review to evaluate the local control
and amputation-free survival in patients who received preoperative
radiation therapy prior to undergoing a marginal resection for a soft tissue
sarcoma of the extremity. The authors concluded that patients can expect
excellent rates of local control and limb preservation regardless of whether
they have a marginal, wide, or radical resection according to the classic
Enneking margin definitions [37].”](https://image.slidesharecdn.com/softtissuetumor-160706134441/85/Soft-tissue-tumor-31-320.jpg)